Prostate Cancer: Perspectives on Therapeutic Advances

Dr. Jim C. Hu
“The advent of robotically assisted and minimally invasive surgical practices, along with newer imaging approaches, has dramatically transformed treatment options for patients with prostate cancer,” says Jim C. Hu, MD, MPH, Director of The Lefrak Center for Robotic Surgery at NewYork-Presbyterian/Weill Cornell Medical Center. A urologic oncologist and one of the world’s leading experts in robotic surgery, Dr. Hu has performed thousands of robot-assisted surgeries for urologic cancers and benign disease and has developed many technical modifications and refinements to the procedures that effectively safeguard surrounding tissues and nerves during the surgery. Dr. Hu also pursues important work in new technology-enabled approaches that include partial gland or focal prostate cancer treatment and cryotherapy.
As Director of The Lefrak Center, Dr. Hu spearheads clinical and research initiatives in urologic oncology and collaborates with colleagues in Weill Cornell Medicine’s Sandra and Edward Meyer Cancer Center. “My goal is to advance treatments with the intention of decreasing morbidity and improving the effectiveness of cancer control,” says Dr. Hu. “Our research needs to look critically at why we do the things we do and whether or not it actually makes a difference in outcomes.”
Emerging Role of Partial Gland Ablation
“The perception that prostate cancer is overdiagnosed and over-treated remains,” notes Dr. Hu. “That is probably why PSA testing continues to be enveloped in controversy, but also why focal therapy is becoming more widely accepted to treat localized prostate cancer. High intensity focused ultrasound (HIFU) and cryotherapy enable us to preserve noncancerous prostate tissue and minimize damage to surrounding healthy tissue or organs, providing the potential for better functional outcomes.”
HIFU for the treatment of prostate cancer is in its early stages of use in the U.S. The approach uses an ultrasound-guided transducer to ablate the cancerous tissue. The method is radiation-free and offers significantly lower risk of side effects than radiation therapy.
Prior to November 2015, HIFU was not FDA approved in this country for focal therapy. “American men who wanted to undergo the procedure would need to travel to Mexico, Canada, or Europe, where these devices were readily available,” says Dr. Hu.
In 2015, the FDA approved HIFU for the ablation of prostate gland tissue, but not for a prostate cancer indication, citing there was not enough long-term evidence for efficacy or patient benefit. In fact, a review of studies undertaken by Dr. Hu and colleagues in the field supports this concern.
“In the review paper we looked at all of the publications that reference HIFU,” notes Dr. Hu. “There were only 12 papers from a handful of international centers that have been using the procedure.” The investigators reported that early evidence suggests that partial gland ablation is a safe treatment option for men with localized disease. However, longer-term studies are needed to evaluate its efficacy and functional outcomes, to be able to identify optimal candidates for this therapy, and to provide data that will allow for better comparison between studies and among treatment modalities.
Dr. Hu sees HIFU as a potentially promising therapy and offers the procedure to patients in his practice. “Some men may find value in undergoing HIFU to focally treat areas of prostate cancer and delay surgical or whole-gland irradiation, which have greater risks of erectile dysfunction and urinary incontinence,” says Dr. Hu. “Additionally, men diagnosed with slow-growing cancers may find that HIFU is an ideal treatment to alleviate significant distress and anxiety that often accompany a prostate cancer diagnosis. We want to make sure that we are using new technology such as high-intensity focused ultrasound responsibly, and cataloging the outcomes to make sure they are justifiable in the long term.”
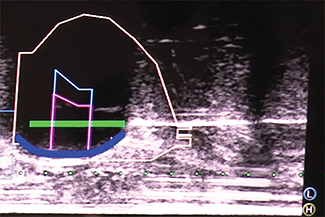
MRI-ultrasound fusion-guided cryotherapy shows the cryotherapy needle (horizontal white line) as it is advanced into the region with cancer. The prostate is outlined in a thin white line; the lesion is outlined in pink. The blue line represents the edge of the ice ball that is monitored under real-time ultrasound.
Courtesy of Dr. Jim C. Hu.
An alternative to HIFU for focal therapy is cryotherapy, which destroys the cancerous tissue by freezing the cells. Dr. Hu performed the first in-office MRI-ultrasound fusion-guided cryotherapy in New York City and the Northeast.
“Building upon the technology that allows more accurate detection of prostate cancer during biopsy, we use cryotherapy to destroy areas of biopsy-identified prostate cancer with MRI guidance,” says Dr. Hu. “Additionally, we can do this procedure in the office. Patients come in for a 45-minute treatment — no anesthesia is needed — then leave the office and go about their day. This will be a transformative approach for prostate cancer treatment. A benefit compared to HIFU is the real-time monitoring of the area that is being thermally ablated and no limitation in terms of the prostate size. Larger size prostates prohibit the use of HIFU.” Dr. Hu is currently leading an effort with the FDA to implement a registry to enable more in-depth study of prostate ablation.
Robotic Approaches in Prostate Cancer: Tried and True
When Dr. Hu began using robotic technology for the treatment of prostate cancer and other urologic cancers more than a decade ago, less than 10 percent of surgeries for all prostate cancer were being done robotically. As one of the highest volume surgeons in the field at the time, it afforded Dr. Hu the opportunity to explore the technology’s value and ultimate role in depth. Dr. Hu’s work was published in a series of articles, Surgery in Motion, in European Urology. The articles focus on technique and outcomes in robotic-assisted surgeries, and each article is linked to a video of the procedure that records and corroborates for physicians and patients the development of robotic surgery’s efficacy when applied to prostate cancers.
Dr. Hu’s published research has consistently furthered the development of robotic surgery, from a study published in 2008 in the Journal of Endourology on a technique for sparing the neurovascular bundle and consequently a patient’s sexual function, followed by several articles on bladder neck preservation during robotic-assisted laparoscopic radical prostatectomy, and including, most recently, a study published in the Journal of Urology in January 2017 that compares cancer control and survival after robot-assisted to open radical prostatectomy. Today 80 to 90 percent of surgeries for prostate cancer involve robotics.
“I want to convey that we need to be experts in all treatments for prostate cancer, and not let our biases or focused expertise with one treatment dictate what patients should receive,” says Dr. Hu. “In order to provide personalized care, I believe we need different tools to suit each man’s preferences and
disease characteristics. These run the gamut from active surveillance and focal therapy to radical prostatectomy.”
PSA Testing: Its Relevance is Returning
Dr. Hu also has been at the vanguard of empirically examining and confronting controversies that seem to attend advances in the diagnosis of prostate cancer — most notably PSA testing. “In 2008, our field changed dramatically when the U.S. Preventive Services Task Force put forth their recommendation against PSA testing,” notes Dr. Hu. “This reduced the amount of PSA testing, increased active surveillance, and led to greater uptake and demand for MRI-guided biopsy to make sure we accurately sample the prostate to differentiate men who have low-risk cancers that need active surveillance versus those who had more aggressive cancers needing surgical therapy. With the introduction of fusion technologies, MRI-guided biopsy has really taken off. We now have the ability to fuse MRI images onto an ultrasound, superimposing the areas that are abnormal.”
However, the relevance of screening for PSA remained in question and to assess the effect of the Task Force recommendations, Dr. Hu and his colleagues examined data from the Surveillance, Epidemiology, and End Results Program, a National Cancer Institute database. They found that the decline in PSA screening has significantly altered the way prostate cancer now presents: 12 percent of men over 75 were diagnosed with metastatic prostate cancer in 2013, compared with 7.8 percent in 2011. And the proportion of men diagnosed with aggressive cancer increased from 68.9 percent to 72 percent over the same period. The results were published in the May 2017 issue of JAMA Oncology.
“Our study was the first to demonstrate that the incidence of metastatic prostate cancer in older men is rising after reaching an all-time low in 2011,” says Dr. Hu. “The findings suggest a correlation between the increase and the change in prostate cancer screening guidelines recommending against routine PSA testing.”
“It’s what most of us would have predicted, although somewhat sooner,” continues Dr. Hu. “Currently, up to 50 percent of Americans diagnosed with prostate cancer choose active surveillance; however, the implication of our study is that it is important to have the right to choose screening in order to identify whether a patient may have an aggressive or indolent prostate cancer. While in men under 75, there was no change in the rate of prostate cancer metastases, this does not necessarily rule out the value of screening in younger men. The Task Force recommendation came later for younger men. So we might need to watch them over time to see if the data for this population parallels with older men.”
Their study came on the heels of studies published by Dr. Hu and his team in The New England Journal of Medicine in 2016 that showed one of the large, randomized trials that stated PSA testing did not decrease the risk of prostate cancer was flawed.
In April 2017, the U.S. Preventive Services Task Force updated its position on PSA screening, issuing a draft of a revised recommendation statement that advises that clinicians discuss with their patients the potential benefits and harms of PSA-based screening for prostate cancer in men ages 55 to 69 years and that the decision whether to be screened should be an individual one. Final recommendations by the Task Force are pending based on their review of public comments to the draft.
Reference Articles
Hu JC, Nguyen P, Mao J, Halpern J, Shoag J, Wright JD, Sedrakyan A. Increase in prostate cancer distant metastases at diagnosis in the United States. JAMA Oncology. 2017 May 1;3(5):705-07.
Golan R, Bernstein AN, McClure TD, Sedrakyan A, Patel NA, Parekh DJ, Marks LS, Hu JC. Partial gland treatment of prostate cancer using high-intensity focused ultrasound in the primary and salvage settings: A systematic review. The Journal of Urology. 2017 Apr 19. [Epub ahead of print]
McClure TD, Margolis DJ, Hu JC. Partial gland ablation in the management of prostate cancer: A review. Current Opinion in Urology. 2017 Mar;27(2):156-60.
Halpern JA, Shoag JE, Artis AS, Ballman KV, Sedrakyan A, Hershman DL, Wright JD, Shih YC, Hu JC. National trends in prostate biopsy and radical prostatectomy volumes following the US Preventive Services Task Force Guidelines Against Prostate-Specific Antigen Screening. JAMA Surgery. 2017 Feb 1;152(2):192-98.
Hu JC, O’Malley P, Chughtai B, Isaacs A, Mao J, Wright JD, Hershman D, Sedrakyan A. Comparative effectiveness of cancer control and survival after robot-assisted versus open radical prostatectomy. The Journal of Urology. 2017 Jan;197(1):115-21.
Shoag JE, Mittal S, Hu JC. More on reevaluating PSA testing rates in the PLCO Trial. The New England Journal of Medicine. 2016 Oct 13;375(15):1500-01.
Hu JC, Laviana A, Sedrakyan A. High-intensity focused ultrasound for prostate cancer: Novelty or innovation? JAMA. 2016 Jun 28;315(24):2659-60.
Shoag JE, Mittal S, Hu JC. Reevaluating PSA testing rates in the PLCO Trial. The New England Journal of Medicine. 2016 May 5;374(18):1795-96.
Related Publications
A Dedicated Team Focuses on Urinary Disorders
Urology: A Focus on Faculty 2017 Issue 2