Rehabilitation Medicine: At the Front Line of Spine Care
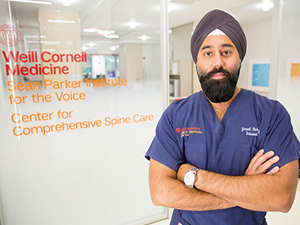
Dr. Jaspal Ricky Singh
In 2016, Weill Cornell Medicine launched the Center for Comprehensive Spine Care, enabling patients to receive highly skilled, interdisciplinary treatment for spinal conditions in one dedicated location. Emphasizing the importance of providing patients with access to both nonoperative and surgical expertise, the Center is co-directed by Jaspal Ricky Singh, MD, who is triple-boarded in Physical Medicine and Rehabilitation, Sports Medicine, and Pain Medicine and also serves as Director of Interventional Spine in the Department of Rehabilitation Medicine at NewYork-Presbyterian/ Weill Cornell Medical Center, and Roger Härtl, MD, Director of Spinal Surgery and Neurotrauma in Weill Cornell’s Department of Neurological Surgery. They lead a team of spine specialists from rehabilitation medicine, physical therapy, neurology, neurosurgery, and anesthesiology.
Rehabilitation medicine specialists are at the front line of treatment in the Center for Comprehensive Spine Care, performing comprehensive physical examinations to develop a differential diagnosis and to determine if conservative methods are appropriate or if the patient requires a surgical consult. Only about 10 percent of spine patients will go on to surgery.
“In our dedicated spine center, physiatrists can serve as the front line for evaluating patients’ spine disorders, referring them to surgeons and other specialists, if needed, for consultation on the same day.” — Dr. Jaspal R. Singh
Importance of Interdisciplinary Perspectives
The heterogeneous nature of spine disorders necessitates an interdisciplinary perspective and treatment strategy that includes conservative management alone or in concert with surgical approaches. “The majority of spine patients have conditions that are benign and self-limited. These patients will likely not become surgical candidates, but they do require treatment,” says Dr. Singh. “The most successful outcomes for spine patients are derived from the insights, experience, and expertise of a team of practitioners who consult with each other to address all aspects of the patient’s spinal disease and pathology. These include pain, disability, and overall quality of life.”
Traditionally, spine care is driven by which specialist — neurologist, surgeon, physiatrist, pain medicine physician — sees the patient first. By reviewing cases together, team members in the Center for Comprehensive Spine Care examine spine issues from an integrative approach, identifying the specific causes of a patient’s condition and developing targeted therapies together that will best serve the patient’s individual circumstances.
“For example, not all spinal stenosis is the same,” says Dr. Singh. “Is it a soft disc herniation, which can sometimes reabsorb? Is it a bone segment that’s not going to reabsorb? Is that person’s neck stable? All these factors are taken into consideration to prognosticate how a person is expected to do and when, if ever, it is necessary to intervene aggressively to prevent neurological injury. The result of this interdisciplinary approach is a coordination of services that optimizes the experience of our patients and the outcomes of their care.
“A great advantage of our center is that now we are all co-located in one center,” continues Dr. Singh. “If I have tried some conservative measures for a patient’s spine issue — medication, physical therapy, an interventional procedure — and they are still not progressing, I can schedule a surgical consultation quickly. In fact, there have been patients who’ve gone from seeing me to coordinating and planning a surgery in the same day.”
Pain Management: A Multimodality Approach
“Rehabilitation medicine doesn’t only determine what is causing spine pain, but equally important, focuses on helping our patients return to the activities they love and the tasks they need to do,” says Michael T. Sein, MD, a physiatrist fellowship trained in pain medicine and a member of the Center for Comprehensive Spine Care.

Dr. Michael T. Sein
Drs. Singh, Sein, and their colleagues employ a multidisciplinary approach to treating pain by integrating physical therapy and interventional pain management techniques and individualizing treatment plans with a focus on functional restoration. “We provide whatever form of therapy is best for that patient,” says Dr. Sein. “The data has become clear that there are very real risks to chronic opioid use, so we have to figure out what we can offer in their place. This includes multimodal treatments that do not rely on one, single approach. You have to create a multi-tiered plan that may include medication, rehabilitation therapy, or interventional procedures in order to relieve suffering and reestablish quality of life.”
“We provide pain management for patients who find it difficult to complete physical therapy or for those who were not helped by physical therapy, those patients with a history of chronic pain who may need additional pain relief in order to undergo surgery, and for those who have not been helped by surgery,” says Dr. Singh. “In addition to incorporating medications to manage inflammation or neuropathic pain, our pain specialists also work with a number of novel compounds unique to pain management.”

Team members also provide a range of minimally invasive procedures to target and alleviate the causes of chronic pain, especially for patients in whom medications have failed. Their expertise includes nerve blocks, injections, intrathecal pump therapy, and radiofrequency ablation. They are also among the most experienced in spinal cord stimulation and neuromodulation, a technique that uses electrical stimulation or delivers pharmaceutical agents directly to a target area to modify how the nerves conduct pain signals.
“Advances in technology, such as musculoskeletal ultrasound, allow physicians to perform procedures in the office that have been previously limited to the operating room or procedure suite,” adds Dr. Sein. “We are now able to visualize nerves and blood vessels in a way that we couldn’t do purely with fluoroscopy. As ultrasound imaging improves in resolution and portability so does our ability to intervene in a safe and effective manner right at the bedside. The advances in technology that translate to patient care do not occur in a vacuum at a research facility; we’re taking those advances and putting them into action.”
Among their current research initiatives, the Center’s rehabilitation medicine physicians are evaluating the safety and efficacy of growth factors and stem cells in the treatment of facet and sacroiliac joint pain. In addition, they are working with basic scientists to develop a safe epidural injection consisting of these growth factors.
“The Spine Center is all about optimizing the patient experience,” says Dr. Singh. “The speed in which patients can be seen by the appropriate practitioner has been increased dramatically. We have a great group of specialists — and though we all see patients a little differently, each of us brings our expertise to the table to develop the most appropriate treatment plan for each patient.”
Reference Articles
Mehta P, Syrop I, Singh JR, Kirschner J. Systematic review of the efficacy of particulate versus nonparticulate corticosteroids in epidural injections. PM&R. 2017 May;9(5):502-12.
Singh JR, Cardozo E, Christolias GC. The clinical efficacy for two-level transforaminal epidural steroid injections. PM&R. 2017. Apr;9(4):377-82.
Related Publications





