Strategic and Multipronged Approaches to Spinal Tumors
NewYork-Presbyterian is among the most advanced centers in the nation for the diagnosis and treatment of both primary and metastatic tumors of the spine. The brain and spine tumor programs at NewYork-Presbyterian/Weill Cornell Medical Center and NewYork-Presbyterian/Columbia University Irving Medical Center integrate multiple disciplines to provide comprehensive treatment strategies that include minimally invasive surgery, radiation therapies, and intra-arterial chemotherapy. While surgery remains the cornerstone of treatment for pain, instability, and improved neurological function, today a number of options and alternatives have emerged from the medical, interventional radiology, and radiation oncology fields that are offering patients better outcomes and prolonged quality of life.
Detecting Tumors Sooner and Smaller

Dr. Paul C. McCormick
Neurosurgeon Paul C. McCormick, MD, MPH, Director of The Spine Hospital at the Neurological Institute of New York at NewYork-Presbyterian/Columbia, is a world-renowned expert in the microsurgical management of spinal tumors and vascular malformations. In his more than 25-year career at Columbia, Dr. McCormick has performed nearly 7,000 spinal procedures for patients from around the world.
Dr. McCormick has a particular interest in benign tumors located both inside and outside of the spinal cord. In the 1990s, he served as lead author in the development of a classification system for the clinical evaluation and correlation of risk with respect to surgery of spinal cord tumors. The McCormick Classification System, which remains in use today, grades the clinical severity of spinal cord tumors. “We developed the classification for intramedullary spinal cord tumors that has allowed us to define and determine appropriate treatment modalities for patients,” says Dr. McCormick. “Part of the point of establishing the system was that in years past, patients’ diagnosis would be delayed because we didn’t have the precision of imaging. Tumors were larger, and patients were not in good neurologic condition. The larger the tumor, the more impaired the patient would be.”
“The improved sensitivity, specificity, and availability of imaging have allowed us to diagnose tumors at a much earlier stage now and have also lessened the risk of surgery.”
— Dr. Paul C. McCormick
“The improved sensitivity, specificity, and availability of imaging have allowed us to diagnose tumors at a much earlier stage now and have also lessened the risk of surgery,” continues Dr. McCormick. “We’ve also moved forward in terms of our techniques, procedures, and technology.”
Dr. McCormick notes that with the advent of more precise imaging, including MRI, physicians are also seeing very small tumors that are clearly incidental in nature in patients who are not symptomatic. “This has created a dilemma as to what to do for these patients,” says Dr. McCormick. “It’s a burden for patients to know that they have a tumor. If it’s a malignancy, however, the earlier you treat something the more likely you are to be able to cure or at least manage it. With benign tumors in patients who are not symptomatic, you can’t make them better than they already are.”
Dr. McCormick and his Columbia colleagues typically do not offer surgery to patients who are asymptomatic. “It may be another 5, 10, or 20 years before these tumors grow to a point where they begin to cause symptoms,” he says. “So, you can maintain a patient with normal neurologic function for many years. You don’t have to treat the MRI, so to speak.”
Benign spinal cord tumors represent a small percentage of the overall spinal oncology program at Columbia, says Dr. McCormick.“Treatment for malignant metastatic tumors that affect the spinal column itself requires a team effort,” says Dr. McCormick, who frequently collaborates with Andrew B. Lassman, MD, Chief of Neuro-Oncology, and Simon Cheng, MD, a radiation oncologist. “It is critically important — especially from a patient’s standpoint — to have leaders in these fields evaluating and recommending appropriate treatment plans. We work closely together to achieve the best outcomes for our patients.”
Navigating the Complexities of Spine Oncology
Neurosurgeon Ali A. Baaj, MD, of the Department of Neurological Surgery at NewYork-Presbyterian/Weill Cornell, specializes in spinal surgery with advanced training and expertise in spinal oncology and complex reconstructive surgery for spinal deformity and scoliosis for both adults and children. Accomplished in both minimally invasive and open complex spine surgery, one of Dr. Baaj’s interests focuses on spinal cord and spinal column pathologies.
“In some cases, these are benign conditions, and in other instances, they are malignant and require a multidisciplinary team in order to evaluate, treat, and manage the patient both surgically and non-surgically,” says Dr. Baaj. “The mainstay of treatment for many of these metastatic diseases involves chemotherapy and radiation therapy and not necessarily surgery. Surgery is not used to cure the disease; it’s used to remove the focal pressure off the spinal cord.”
Dr. Baaj maintains a close relationship with providers in medical oncology, radiation oncology, neuroradiology, and specialists in pain management and rehabilitation medicine. “It is truly a multidisciplinary process when it comes to metastatic disease, the most common condition in the spine oncology world,” says Dr. Baaj, who serves on a tumor board that meets each week to discuss treatment plans for complex cases.
During surgery, Dr. Baaj utilizes neuronavigation tools and intraoperative neuromonitoring. “A technician present in the operating room monitors the function of the nerves and the spinal cord in real time,” he says. “At the same time, that data is being reviewed remotely by a neurologist to ensure that what we’re doing is safe and that we’re not crossing the boundary into normal tissue, remaining focused only on the abnormal tissue.”
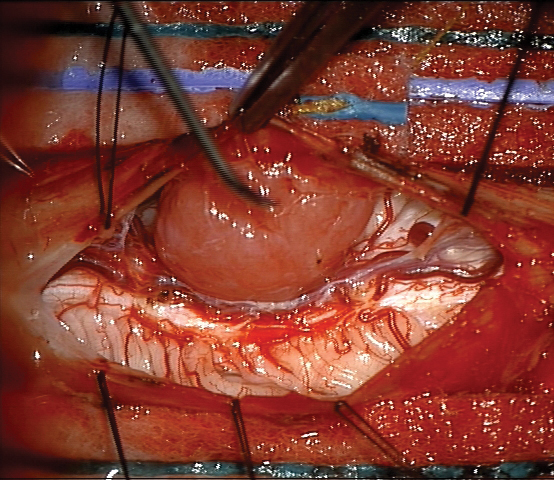
Cervical spine meningioma
“In terms of imaging,” continues Dr. Baaj, “we have close and important interactions with Weill Cornell neuroradiologists, frequently reviewing films together. The type of tumor dictates how much of it we need to resect. We don’t always need to remove entire metastatic tumors, especially where there is extensive tumor infiltration of the spinal column. Many times, we need only to remove the part that’s compressing on the spinal cord and causing neurological dysfunction. This approach minimizes complications.”
As Dr. Baaj explains, pain control and palliation are of utmost importance with spinal oncology specifically related to metastatic disease. “Because many of these conditions are not curable, our goal is to provide the best quality of life for patients with excellent pain control. We do that with surgery and non-surgical interventions, such as systemic therapy and radiation oncology with the assistance of the palliative pain service, to make sure that the patient isn’t suffering.”
“We don’t always need to remove entire metastatic tumors, especially where there is extensive tumor infiltration of the spinal column. Many times, we need only to remove the part that’s compressing on the spinal cord and causing neurological dysfunction. This approach minimizes complications.”
— Dr. Ali A. Baaj
Although most of Dr. Baaj’s work in spinal oncology involves metastatic spine disease, he also treats a significant portion of benign spine tumors as well. “These intramedullary tumors, which involve the spinal cord itself or the area just outside of the spinal cord, are very challenging to treat,” he says. “They’re difficult to resect technically, requiring microsurgical skills. However, in some instances, patients can receive a total cure after surgical resection. Those types of tumors provide for some successful outcomes and very happy patients.”
Targeting Tumors with Stereotactic Radiosurgery
Susan C. Pannullo, MD, Director of Neuro-Oncology and Neurosurgical Radiosurgery in the Department of Neurological Surgery at NewYork-Presbyterian/Weill Cornell, is one of the few physicians in the world who is board certified in both neurology and neurological surgery, and perhaps the only one also fellowship trained in neuro-oncology.
“My role on this team is to provide patients with stereotactic radiosurgery procedures, which can be useful not only by shrinking tumors, but also by helping patients with symptoms from spine tumors, such as pain or weakness,” says Dr. Pannullo. “Patients often will have surgery first and then we’ll do radiosurgery, targeting remaining visible tumor or microscopic tumor cells that may be left behind after the surgery.”
“If we consider cancer more like diabetes or high blood pressure where we don’t have a cure, but we have management options that can help patients live with excellent quantity and quality of life, we can more effectively create optimal customized treatment plans to approach effects of cancer such as brain and spine metastases.”
— Dr. Susan C. Pannullo
Occasionally, when tumors are found early and are not encroaching upon the spinal cord or the spinal nerves, Dr. Pannullo uses stereotactic radiosurgery to manage definitively the tumor and inhibit its further growth, as well as to manage the pain that can come from tumors replacing the normal elements of the spine.
“Stereotactic radiosurgery, unlike the older forms of radiation for spinal tumors, is very focused,” explains Dr. Pannullo. “Years ago, and still now in some situations, a larger blanket of radiation was provided to the area involved with the tumor and the area surrounding it. Now, we prefer to limit radiation to just the area involved with the tumor in order to minimize the dose of radiation that goes to normal surrounding tissues, such as the spinal cord, spinal nerves, and nearby organs. In addition, patients who are receiving chemotherapy may have a need to preserve the normal bone marrow in the surrounding spinal bones. So, we limit the amount of radiation delivered to adjacent, normal spinal segments so as to lessen the impact upon the bone marrow, which is needed to create the normal blood cells that are reduced in number by the chemotherapy. Advances in the field have enabled us to refine this technique over the past few years to the point where we can be extremely precise and perform the treatment with little or no discomfort to the patient.”
Dr. Pannullo stresses the importance of modern communication that enables the care team to rapidly coordinate care for patients. “With a single email, I can pull in multiple specialists in order to coordinate a treatment plan and patient appointments, often within minutes,” she says. “For a patient who has a compelling and complicated problem like a spinal metastasis, this type of rapid deployment of expertise and resources is particularly crucial.”
“Patients who have spine metastases should be approached in a strategic and thoughtful way with a long-term view of quality of life and long-term side effects of treatments,” adds Dr. Pannullo. “If we consider cancer more like diabetes or high blood pressure where we don’t have a cure, but we have management options that can help patients live with excellent quantity and quality of life, we can more effectively create optimal customized treatment plans to approach effects of cancer such as brain and spine metastases.”
Managing Symptoms with Less Invasive Interventions

Dr. Athos Patsalides
Athos Patsalides, MD, MPH, an interventional neuroradiologist in the Department of Neurological Surgery at NewYork-Presbyterian/Weill Cornell, practices in a rapidly evolving subspecialty that offers minimally invasive image-guided procedures for spinal tumors. “My role is to provide percutaneous treatments that specifically target the spinal tumor or spinal metastasis in terms of pain or tumor control,” says Dr. Patsalides. “When a patient has a tumor anywhere in the spine that is causing significant pain and/or pathologic vertebral compression fractures, we can offer vertebral augmentation. In vertebroplasty, we inject a cement mixture into the fractured bone to restore bone integrity. We can also perform kyphoplasty by inserting a balloon into the fractured bone to create a space and then fill it with cement.”
Dr. Patsalides also performs fluoroscopic-guided thermal radio-frequency ablation for nonresectable spinal tumors. “The purpose of ablation, which also includes cryoablation and microwave ablation, is to treat at least part of the tumor and offer tumor control. It is a minimally invasive percutaneous procedure that involves the placement of a needle through a very small incision in the back and into the tumor in the spine with little trauma to the patient,” says Dr. Patsalides. “Often we do kyphoplasty and ablation together in a single session when the patient has a very painful metastasis that is causing a fracture in the spine. The patient goes home on the same day and the recovery process is minimal.”
“Spinal intra-arterial chemotherapy is a unique, therapeutic treatment developed here at Weill Cornell — the only hospital where this procedure is performed — which is given to carefully selected patients who are at risk for paralysis from spinal cord compression.”
— Dr. Athos Patsalides
When standard treatments, such as radiation and systemic chemotherapy, have failed, Dr. Patsalides can deliver chemotherapy directly to the tumor through a catheter inserted into the femoral artery that supplies blood to the tumor. “Spinal intra-arterial chemotherapy is a unique, therapeutic treatment developed here at Weill Cornell — the only hospital where this procedure is performed. The treatment is used with carefully selected patients who are at risk for paralysis from spinal cord compression,” he explains. “We don’t do this very often, thankfully, because most patients respond to the standard treatments.”
Dr. Patsalides and his colleagues tested this novel treatment in a Phase 1 clinical trial of nine patients with progressive spinal metastatic disease and cord compression. All of the patients had metastatic disease from solid organs and were not candidates for further radiation therapy or surgery. A total of 19 spinal intra-arterial chemotherapy (SIAC) procedures were performed, and the follow-up period ranged from one to seven months. Local tumor control was seen in eight of the nine patients. The preliminary results of this study, which were published in the Journal of Neurosurgery: Spine in 2016, support the hypothesis that SIAC is feasible and safe. The clinical trial is ongoing with completion slated for early 2021.
“We showed that this minimally invasive approach can stop the tumor progression by directing chemotherapy into the arteries that supply the tumor,” says Dr. Patsalides, noting that some 20 patients have been successfully treated with this approach to date. “This is also a nontraumatic outpatient procedure without any significant or adverse effects to the patient.”
Dr. Patsalides is optimistic that the future will bring more minimally invasive approaches that will target spinal tumors, and at the same time will not compromise other treatments that patients are receiving. “We’ve made a lot of progress in the last two years, and I believe there are going to be many more options soon.”
Reference Article
Patsalides A, Yamada Y, Bilsky M, Lis E, Laufer I, Gobin YP. Spinal intra-arterial chemotherapy: Interim results of a Phase 1 clinical trial. Journal of Neurosurgery: Spine. 2016 Feb;24(2):217-22.
Related Publications

Dr. Cigdem Akman Leads Child Neurology at Columbia




