Health Library
Merkel Cell Carcinoma Treatment (PDQ®): Treatment - Health Professional Information [NCI]
- General Information About Merkel Cell Carcinoma
- Cellular Classification of Merkel Cell Carcinoma
- Stage Information for Merkel Cell Carcinoma
- Treatment Option Overview for Merkel Cell Carcinoma
- Treatment of Stage I and II Merkel Cell Carcinoma
- Treatment of Stage III Merkel Cell Carcinoma
- Treatment of Stage IV Merkel Cell Carcinoma
- Treatment of Recurrent Merkel Cell Carcinoma
- Latest Updates to This Summary (04 / 19 / 2024)
- About This PDQ Summary
General Information About Merkel Cell Carcinoma
Merkel cell carcinoma (MCC) was originally described by Toker in 1972 as trabecular carcinoma of the skin.[1] Other names for MCC include Toker tumor, primary small cell carcinoma of the skin, primary cutaneous neuroendocrine tumor, and malignant trichodiscoma.[2]
MCC is an aggressive neuroendocrine carcinoma arising in the dermoepidermal junction (see Figure 1), and it is the second most common cause of skin cancer death after melanoma.[3,4] Although the exact origin and function of the Merkel cell remains under investigation, it is thought to have features of both epithelial and neuroendocrine origin and arise in cells with touch-sensitivity function (mechanoreceptors).[5,6,7,8,9,10,11]
Therapeutic options have been historically limited for patients with advanced disease; however, new immunotherapeutic approaches are associated with durable responses.[12]
Anatomy

Figure 1. Merkel Cell Anatomy.
Incidence and Mortality
MCC incidence increases progressively with age. There are few cases in patients younger than 50 years, and the median age at diagnosis is about 65 years (see Figure 2).[13] Incidence is considerably greater in White individuals than in Black individuals and slightly greater in men than in women.[13,14,15,16,17]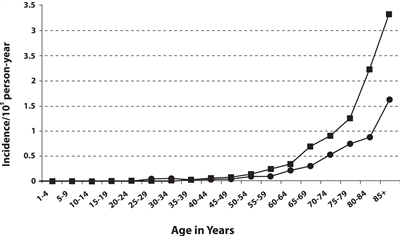
Figure 2. Frequency of MCC by age and sex of men (square) and women (circle). Reprinted from Journal of the American Academy of Dermatology, 49 (5), Agelli M and Clegg L, Epidemiology of primary Merkel cell carcinoma in the United States, pp. 832–41, Copyright (2003), with permission from Elsevier.
MCC occurs most frequently in sun-exposed areas of skin, particularly the head and neck, followed by the extremities, and then the trunk.[5,16,18] Incidence has been reported to be greater in geographic regions with higher levels of ultraviolet B sunlight.[16]
As of 2013, MCC had an annual incidence of 0.7 cases per 100,000 people in the United States.[19] The incidence has been increasing over the past several decades, almost doubling in the United States between 2000 and 2013. This rise is potentially related to more accurate diagnostic pathology tools, improved clinical awareness of MCC, an aging population, increased sun exposure in susceptible populations, and improved registry tools. The incidence is also higher in immunosuppressed populations (HIV, hematologic malignancies, immunosuppressive medications, etc.).[20] Approximately 25,000 cases of MCC have been recorded in the United States since 2000, including more than 2,200 incident cases reported in 2014 to the National Program of Cancer Registries/SEER combined registries, which captures more than 98% of the U.S. population and the ten most common sites of MCC (see Table 1).[17]
| Anatomical Site | Cases (%) |
|---|---|
| NOS = not otherwise specified; SEER = Surveillance, Epidemiology, and End Results Program. | |
| a Albores-Saavedra J et al: Merkel cell carcinoma demographics, morphology, and survival based on 3,870 cases: A population-based study. J Cutan Pathol. Reprinted with permission © 2009. Published by Wiley-Blackwell. All rights reserved.[17] | |
| Skin, face | 1,041 (26.9) |
| Skin of upper limb and shoulder | 853 (22.0) |
| Skin of lower limb and hip | 578 (14.9) |
| Skin of trunk | 410 (10.6) |
| Skin of scalp and neck | 348 (9.0) |
| Skin, NOS | 234 (6.0) |
| External ear | 120 (3.1) |
| Eyelid | 98 (2.5) |
| Skin of lip | 91 (2.4) |
| Unknown primary site | 31 (0.8) |
| Total | 3,804 (98.3) |
In various cases series, up to 97% of MCCs arise in the skin. MCC primaries in other sites were very rare, as were MCCs from unknown primary sites.[17]
SEER registry data have shown excess risk of MCC as a first or second cancer in patients with several primary cancers.[21] National cancer registries from three Scandinavian countries have identified a variety of second cancers diagnosed after MCC.[22]
Pathogenesis
Increased incidence of MCC has also been seen in people treated heavily with methoxsalen (psoralen) and ultraviolet A (PUVA) for psoriasis (3 of 1,380 patients, 0.2%). This has also been seen in individuals with chronic immune suppression, especially from chronic lymphocytic leukemia, HIV, and previous solid organ transplant.[16,23]
In 2008, a novel polyomavirus (Merkel cell polyoma virus [MCPyV]) was first reported in MCC tumor specimens,[24] a finding subsequently confirmed in other laboratories.[25,26,27] High levels of viral DNA and clonal integration of the virus in MCC tumors have also been reported, [28] along with expression of certain viral antigens in MCC cells and the presence of antiviral antibodies. Not all cases of MCC appear to be associated with MCPyV infection.[29]
MCPyV has been detected at very low levels in normal skin distant from the MCC primary tumor, in a significant percentage of patients with non-MCC cutaneous disorders, in normal-appearing skin in healthy individuals, and in nonmelanoma skin cancers in immune-suppressed individuals.[10,30,31,32] Various methods have been used to identify and quantify the presence of MCPyV in MCC tumor specimens, other non-MCC tumors, blood, urine, and other tissues.[33,34]
The significance of the new MCPyV findings remains uncertain. The prognostic significance of viral load, antibody titer levels, and the role of underlying immunosuppression in hosts (from disease and medications) are under investigation.
Prevalence of MCPyV appears to differ between MCC patients in the United States and Europe versus Australia. There may be two independent pathways for the development of MCC: one driven by the presence of MCPyV, and the other driven primarily by sun damage, especially as noted in patient series from Australia.[25,29,35]
Although no unique marker for MCC has been identified, a variety of molecular and cytogenetic markers of MCC have been reported.[7,10,36]
Clinical Presentation
MCC usually presents as a painless, indurated, solitary dermal nodule with a slightly erythematous to deeply violaceous color, and rarely, an ulcer. MCC can infiltrate locally via dermal lymphatics, resulting in multiple satellite lesions. Because of its nonspecific clinical appearance, MCC is rarely suspected before a biopsy is performed.[5] Photographs of MCC skin lesions illustrate its clinical variability.[37]
A mnemonic [18] summarizing typical clinical characteristics of MCC has been proposed:
AEIOU
- A = Asymptomatic.
- E = Expanding rapidly.
- I = Immune suppressed.
- O = Older than 50 years.
- U = UV-exposed skin.
Not all patients have every element in this mnemonic; however, in this study, 89% of patients met three or more criteria, 52% met four or more criteria, and 7% met all five criteria.[18]
Initial Clinical Evaluation
Because local-regional spread is common, newly diagnosed MCC patients require a careful clinical examination that includes looking for satellite lesions and regional nodal involvement.
Tailoring an imaging work-up to the clinical presentation and any relevant signs and symptoms should be considered. There has been no systematic study of the optimal imaging work-up for newly diagnosed patients, and it is not clear if all newly diagnosed patients, especially those with the smallest primary tumors, benefit from a detailed imaging work-up.
If an imaging work-up is performed, it may include a computed tomography (CT) scan of the chest and abdomen to rule out primary small cell lung cancer as well as distant and regional metastases. Imaging studies designed to evaluate suspicious signs and symptoms may also be recommended. In one series, CT scans had an 80% false-negative rate for regional metastases.[38] Head and neck presentations may require additional imaging. Magnetic resonance imaging has been used to evaluate MCC but has not been studied systematically.[39] Fluorine F 18-fludeoxyglucose positron emission tomography results have been reported in selected cases.[40,41] Baseline routine blood work has been recommended but has not been studied systematically. There are no known circulating tumor markers specifically for MCC.
Initial Staging Results
The results of initial clinical staging of MCC vary widely in the literature, based on retrospective case series reported over decades. For invasive cancers, 48.6% were localized, 31.1% were regional, and 8.2% were distant.[17]
MCC that presents in regional nodes without an identifiable primary lesion is found in a minority of patients, with the percent of these cases varying among the reported series. Tumors without an identifiable primary lesion have been attributed to either spontaneous regression of the primary or metastatic neuroendocrine carcinoma from a clinically occult site.[8,17,18,42,43]
Clinical Progression
In a review of patients from 18 case series, 279 of 926 patients (30.1%) developed local recurrence during follow-up, excluding those presenting with distant metastatic disease. These events have been typically attributed to inadequate surgical margins and/or a lack of adjuvant radiation therapy. In addition, 545 of 982 patients (55.5%) had lymph node metastases at diagnosis or during follow-up.[8]
In the same review of 18 case series, the most common sites of distant metastases were distant lymph nodes (60.1%), distant skin (30.3%), lung (23.4%), central nervous system (18.4%), and bone (15.2%).[8] Many other sites of disease have also been reported, and the distribution of metastatic sites varies among case series.
In one series of 237 patients presenting with local or regional disease, the median time-to-recurrence was 9 months (range, 2–70 months). Ninety-one percent of recurrences occurred within 2 years of diagnosis.[44]
Potential Prognostic Factors
The extent of disease at presentation may provide the most useful estimate of prognosis.[7]
Diagnostic procedures, such as sentinel lymph node biopsy, may help distinguish between local and regional disease at presentation. One-third of patients who lack clinically palpable or radiologically visible nodes will have microscopically evident regional disease.[38] Nodal positivity may be substantially lower among patients with small tumors (e.g., ≤1.0 cm).[45]
Many retrospective studies have evaluated the relationship of a wide variety of biological and histological factors to survival and local-regional control.[7,8,17,38,44,46,47,48,49,50,51,52,53,54,55,56,57][Level of evidence C2] Many of these reports are confounded by small numbers, potential selection bias, referral bias, short follow-up, no uniform clinical protocol for both staging and treatment, and are underpowered to detect modest differences.
A large, single-institution, retrospective study of 156 patients with MCC, with a median follow-up of 51 months (range, 2–224 months), evaluated histological factors potentially associated with prognosis.[55][Level of evidence C1] Although this report was subject to potential selection and referral bias, both univariate and multivariate analyses demonstrated a relationship between improved cause-specific survival and circumscribed growth pattern versus infiltrative pattern, shallow-tumor depth versus deep-tumor depth, and absence of lymphovascular invasion versus presence of lymphovascular invasion. Adoption of these findings into a global prognostic algorithm awaits independent confirmation by adequately powered studies.
A 2009 study investigated whether the presence of newly identified MCPyV in MCC tumor specimens influenced clinical outcome among 114 Finnish patients with MCC. In this small study, patients whose tumors were MCPyV positive appeared to have better survival than patients whose tumors were MCPyV negative.[58][Level of evidence C2] Standardization of procedures to identify and quantify MCPyV and relevant antibodies is needed to improve understanding of both prognostic and epidemiological questions.[10]
Prognosis
The most significant prognostic parameters for MCC include tumor size and the presence of locoregional or distant metastases. These factors form the basis of the American Joint Committee on Cancer staging system for MCC.[59,60] Although an increasing primary tumor size correlates with an increased risk of metastatic disease, MCC tumors of any size have significant risk of occult metastasis, supporting the use of sentinel lymph node biopsy for all cases.[61] Additional features of the primary tumor, such as lymphovascular invasion and tumor growth pattern, may also have prognostic significance. Clinically detectable nodal disease is associated with worse outcome than microscopic metastases.[55,59] Other findings associated with worse prognosis include sheet-like involvement in lymph node metastases and an increasing number of metastatic lymph nodes.[60,62]
The bulk of MCC literature is from small case series, which are subject to many confounding factors. For this reason, the relapse and survival rates reported by stage vary widely in the literature. In general, lower-stage disease is associated with better overall survival.[63] For more information, see the Potential Prognostic Factors section.
Outcomes from patients presenting with small volume local disease and pathologically confirmed cancer-negative lymph nodes report a cause-specific 5-year survival rate exceeding 90% in one report.[44,55][Level of evidence C2]
A tabular summary of treatment results of MCC from 12 series illustrates the difficulty in comparing outcome data among series.[7]
Using the SEER Program registry MCC staging system adopted in 1973, MCC survival data (1973–2006) by stage is summarized in Figure 3.[17]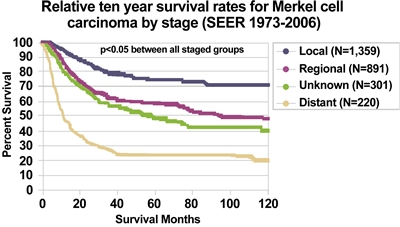
Figure 3. Relative ten-year survival rates for Merkel Cell Carcinoma by stage (SEER 1973–2006). Albores-Saavedra J et al: Merkel cell carcinoma demographics, morphology, and survival based on 3,870 cases: A population-based study. J Cutan Pathol. Reprinted with permission © 2009. Published by Wiley-Blackwell. All rights reserved.
References:
- Toker C: Trabecular carcinoma of the skin. Arch Dermatol 105 (1): 107-10, 1972.
- Schwartz RA, Lambert WC: The Merkel cell carcinoma: a 50-year retrospect. J Surg Oncol 89 (1): 5, 2005.
- Agelli M, Clegg LX, Becker JC, et al.: The etiology and epidemiology of merkel cell carcinoma. Curr Probl Cancer 34 (1): 14-37, 2010 Jan-Feb.
- Harms PW: Update on Merkel Cell Carcinoma. Clin Lab Med 37 (3): 485-501, 2017.
- Nghiem P, McKee PH, Haynes HA: Merkel cell (cutaneous neuroendocrine) carcinoma. In: Sober AJ, Haluska FG, eds.: Skin Cancer. BC Decker Inc., 2001, pp 127-141.
- Nghiem P, James N: Merkel cell carcinoma. In: Wolff K, Goldsmith LA, Katz SI, et al., eds.: Fitzpatrick's Dermatology in General Medicine. 7th ed. McGraw-Hill , 2008, pp 1087-94.
- Eng TY, Boersma MG, Fuller CD, et al.: A comprehensive review of the treatment of Merkel cell carcinoma. Am J Clin Oncol 30 (6): 624-36, 2007.
- Medina-Franco H, Urist MM, Fiveash J, et al.: Multimodality treatment of Merkel cell carcinoma: case series and literature review of 1024 cases. Ann Surg Oncol 8 (3): 204-8, 2001.
- Busse PM, Clark JR, Muse VV, et al.: Case records of the Massachusetts General Hospital. Case 19-2008. A 63-year-old HIV-positive man with cutaneous Merkel-cell carcinoma. N Engl J Med 358 (25): 2717-23, 2008.
- Rockville Merkel Cell Carcinoma Group: Merkel cell carcinoma: recent progress and current priorities on etiology, pathogenesis, and clinical management. J Clin Oncol 27 (24): 4021-6, 2009.
- Calder KB, Smoller BR: New insights into merkel cell carcinoma. Adv Anat Pathol 17 (3): 155-61, 2010.
- Cassler NM, Merrill D, Bichakjian CK, et al.: Merkel Cell Carcinoma Therapeutic Update. Curr Treat Options Oncol 17 (7): 36, 2016.
- Agelli M, Clegg LX: Epidemiology of primary Merkel cell carcinoma in the United States. J Am Acad Dermatol 49 (5): 832-41, 2003.
- Hodgson NC: Merkel cell carcinoma: changing incidence trends. J Surg Oncol 89 (1): 1-4, 2005.
- Young JL, Ward KC, Ries LAG: Cancer of rare sites. In: Ries LAG, Young JL, Keel GE, et al., eds.: SEER Survival Monograph: Cancer Survival Among Adults: U. S. SEER Program, 1988-2001, Patient and Tumor Characteristics. National Cancer Institute, 2007. NIH Pub. No. 07-6215, pp 251-61.
- Miller RW, Rabkin CS: Merkel cell carcinoma and melanoma: etiological similarities and differences. Cancer Epidemiol Biomarkers Prev 8 (2): 153-8, 1999.
- Albores-Saavedra J, Batich K, Chable-Montero F, et al.: Merkel cell carcinoma demographics, morphology, and survival based on 3870 cases: a population based study. J Cutan Pathol 37 (1): 20-7, 2010.
- Heath M, Jaimes N, Lemos B, et al.: Clinical characteristics of Merkel cell carcinoma at diagnosis in 195 patients: the AEIOU features. J Am Acad Dermatol 58 (3): 375-81, 2008.
- Paulson KG, Park SY, Vandeven NA, et al.: Merkel cell carcinoma: Current US incidence and projected increases based on changing demographics. J Am Acad Dermatol 78 (3): 457-463.e2, 2018.
- Ma JE, Brewer JD: Merkel cell carcinoma in immunosuppressed patients. Cancers (Basel) 6 (3): 1328-50, 2014.
- Howard RA, Dores GM, Curtis RE, et al.: Merkel cell carcinoma and multiple primary cancers. Cancer Epidemiol Biomarkers Prev 15 (8): 1545-9, 2006.
- Bzhalava D, Bray F, Storm H, et al.: Risk of second cancers after the diagnosis of Merkel cell carcinoma in Scandinavia. Br J Cancer 104 (1): 178-80, 2011.
- Lunder EJ, Stern RS: Merkel-cell carcinomas in patients treated with methoxsalen and ultraviolet A radiation. N Engl J Med 339 (17): 1247-8, 1998.
- Feng H, Shuda M, Chang Y, et al.: Clonal integration of a polyomavirus in human Merkel cell carcinoma. Science 319 (5866): 1096-100, 2008.
- Garneski KM, Warcola AH, Feng Q, et al.: Merkel cell polyomavirus is more frequently present in North American than Australian Merkel cell carcinoma tumors. J Invest Dermatol 129 (1): 246-8, 2009.
- Becker JC, Houben R, Ugurel S, et al.: MC polyomavirus is frequently present in Merkel cell carcinoma of European patients. J Invest Dermatol 129 (1): 248-50, 2009.
- Kassem A, Schöpflin A, Diaz C, et al.: Frequent detection of Merkel cell polyomavirus in human Merkel cell carcinomas and identification of a unique deletion in the VP1 gene. Cancer Res 68 (13): 5009-13, 2008.
- Houben R, Schrama D, Becker JC: Molecular pathogenesis of Merkel cell carcinoma. Exp Dermatol 18 (3): 193-8, 2009.
- Paik JY, Hall G, Clarkson A, et al.: Immunohistochemistry for Merkel cell polyomavirus is highly specific but not sensitive for the diagnosis of Merkel cell carcinoma in the Australian population. Hum Pathol 42 (10): 1385-90, 2011.
- Andres C, Belloni B, Puchta U, et al.: Prevalence of MCPyV in Merkel cell carcinoma and non-MCC tumors. J Cutan Pathol 37 (1): 28-34, 2010.
- Kassem A, Technau K, Kurz AK, et al.: Merkel cell polyomavirus sequences are frequently detected in nonmelanoma skin cancer of immunosuppressed patients. Int J Cancer 125 (2): 356-61, 2009.
- Foulongne V, Dereure O, Kluger N, et al.: Merkel cell polyomavirus DNA detection in lesional and nonlesional skin from patients with Merkel cell carcinoma or other skin diseases. Br J Dermatol 162 (1): 59-63, 2010.
- DeCaprio JA: Does detection of Merkel cell polyomavirus in Merkel cell carcinoma provide prognostic information? J Natl Cancer Inst 101 (13): 905-7, 2009.
- Laude HC, Jonchère B, Maubec E, et al.: Distinct merkel cell polyomavirus molecular features in tumour and non tumour specimens from patients with merkel cell carcinoma. PLoS Pathog 6 (8): , 2010.
- Buck CB, Lowy DR: Immune readouts may have prognostic value for the course of merkel cell carcinoma, a virally associated disease. J Clin Oncol 29 (12): 1506-8, 2011.
- Lemos B, Nghiem P: Merkel cell carcinoma: more deaths but still no pathway to blame. J Invest Dermatol 127 (9): 2100-3, 2007.
- Seattle Cancer Care Alliance: Merkel Cell Carcinoma Information for Patients and Their Physicians: Clinical Photos/Images. Seattle, Wa: Seattle Cancer Care Alliance Skin Oncology Clinic, 2009. Available online. Last accessed April 19, 2024.
- Gupta SG, Wang LC, Peñas PF, et al.: Sentinel lymph node biopsy for evaluation and treatment of patients with Merkel cell carcinoma: The Dana-Farber experience and meta-analysis of the literature. Arch Dermatol 142 (6): 685-90, 2006.
- Anderson SE, Beer KT, Banic A, et al.: MRI of merkel cell carcinoma: histologic correlation and review of the literature. AJR Am J Roentgenol 185 (6): 1441-8, 2005.
- Iagaru A, Quon A, McDougall IR, et al.: Merkel cell carcinoma: Is there a role for 2-deoxy-2-[f-18]fluoro-D-glucose-positron emission tomography/computed tomography? Mol Imaging Biol 8 (4): 212-7, 2006 Jul-Aug.
- Belhocine T, Pierard GE, Frühling J, et al.: Clinical added-value of 18FDG PET in neuroendocrine-merkel cell carcinoma. Oncol Rep 16 (2): 347-52, 2006.
- Missotten GS, de Wolff-Rouendaal D, de Keizer RJ: Merkel cell carcinoma of the eyelid review of the literature and report of patients with Merkel cell carcinoma showing spontaneous regression. Ophthalmology 115 (1): 195-201, 2008.
- Richetta AG, Mancini M, Torroni A, et al.: Total spontaneous regression of advanced merkel cell carcinoma after biopsy: review and a new case. Dermatol Surg 34 (6): 815-22, 2008.
- Allen PJ, Bowne WB, Jaques DP, et al.: Merkel cell carcinoma: prognosis and treatment of patients from a single institution. J Clin Oncol 23 (10): 2300-9, 2005.
- Stokes JB, Graw KS, Dengel LT, et al.: Patients with Merkel cell carcinoma tumors < or = 1.0 cm in diameter are unlikely to harbor regional lymph node metastasis. J Clin Oncol 27 (23): 3772-7, 2009.
- Jabbour J, Cumming R, Scolyer RA, et al.: Merkel cell carcinoma: assessing the effect of wide local excision, lymph node dissection, and radiotherapy on recurrence and survival in early-stage disease--results from a review of 82 consecutive cases diagnosed between 1992 and 2004. Ann Surg Oncol 14 (6): 1943-52, 2007.
- Henness S, Vereecken P: Management of Merkel tumours: an evidence-based review. Curr Opin Oncol 20 (3): 280-6, 2008.
- Skelton HG, Smith KJ, Hitchcock CL, et al.: Merkel cell carcinoma: analysis of clinical, histologic, and immunohistologic features of 132 cases with relation to survival. J Am Acad Dermatol 37 (5 Pt 1): 734-9, 1997.
- Sandel HD, Day T, Richardson MS, et al.: Merkel cell carcinoma: does tumor size or depth of invasion correlate with recurrence, metastasis, or patient survival? Laryngoscope 116 (5): 791-5, 2006.
- Llombart B, Monteagudo C, López-Guerrero JA, et al.: Clinicopathological and immunohistochemical analysis of 20 cases of Merkel cell carcinoma in search of prognostic markers. Histopathology 46 (6): 622-34, 2005.
- Senchenkov A, Barnes SA, Moran SL: Predictors of survival and recurrence in the surgical treatment of merkel cell carcinoma of the extremities. J Surg Oncol 95 (3): 229-34, 2007.
- Goldberg SR, Neifeld JP, Frable WJ: Prognostic value of tumor thickness in patients with Merkel cell carcinoma. J Surg Oncol 95 (8): 618-22, 2007.
- Heath ML, Nghiem P: Merkel cell carcinoma: if no breslow, then what? J Surg Oncol 95 (8): 614-5, 2007.
- Tai P: Merkel cell cancer: update on biology and treatment. Curr Opin Oncol 20 (2): 196-200, 2008.
- Andea AA, Coit DG, Amin B, et al.: Merkel cell carcinoma: histologic features and prognosis. Cancer 113 (9): 2549-58, 2008.
- Paulson KG, Iyer JG, Tegeder AR, et al.: Transcriptome-wide studies of merkel cell carcinoma and validation of intratumoral CD8+ lymphocyte invasion as an independent predictor of survival. J Clin Oncol 29 (12): 1539-46, 2011.
- Fields RC, Busam KJ, Chou JF, et al.: Recurrence and survival in patients undergoing sentinel lymph node biopsy for merkel cell carcinoma: analysis of 153 patients from a single institution. Ann Surg Oncol 18 (9): 2529-37, 2011.
- Sihto H, Kukko H, Koljonen V, et al.: Clinical factors associated with Merkel cell polyomavirus infection in Merkel cell carcinoma. J Natl Cancer Inst 101 (13): 938-45, 2009.
- Harms KL, Healy MA, Nghiem P, et al.: Analysis of Prognostic Factors from 9387 Merkel Cell Carcinoma Cases Forms the Basis for the New 8th Edition AJCC Staging System. Ann Surg Oncol 23 (11): 3564-3571, 2016.
- Iyer JG, Storer BE, Paulson KG, et al.: Relationships among primary tumor size, number of involved nodes, and survival for 8044 cases of Merkel cell carcinoma. J Am Acad Dermatol 70 (4): 637-643, 2014.
- Schwartz JL, Griffith KA, Lowe L, et al.: Features predicting sentinel lymph node positivity in Merkel cell carcinoma. J Clin Oncol 29 (8): 1036-41, 2011.
- Ko JS, Prieto VG, Elson PJ, et al.: Histological pattern of Merkel cell carcinoma sentinel lymph node metastasis improves stratification of Stage III patients. Mod Pathol 29 (2): 122-30, 2016.
- Eng TY, Boersma MG, Fuller CD, et al.: Treatment of merkel cell carcinoma. Am J Clin Oncol 27 (5): 510-5, 2004.



