Health Library
Childhood Melanoma Treatment (PDQ®): Treatment - Patient Information [NCI]
General Information About Childhood Melanoma
Melanoma is a disease in which malignant (cancer) cells form in melanocytes (cells that color the skin).
The skin is the body's largest organ. It protects against heat, sunlight, injury, and infection. Skin also helps control body temperature and stores water, fat, and vitamin D. The skin has several layers, but the two main layers are the epidermis (upper or outer layer) and the dermis (lower or inner layer). Skin cancer begins in the epidermis, which is made up of three kinds of cells:
- Squamous cells: Thin, flat cells that form the top layer of the epidermis.
- Basal cells: Round cells under the squamous cells.
- Melanocytes: Cells that make melanin and are found in the lower part of the epidermis. Melanin is the pigment that gives skin its natural color. When skin is exposed to the sun or artificial light, melanocytes make more pigment and cause the skin to darken.
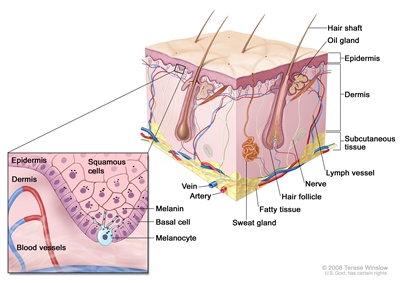
Anatomy of the skin, showing the epidermis, dermis, and subcutaneous tissue. Melanocytes are in the layer of basal cells at the deepest part of the epidermis.
There are different types of cancer that start in the skin.
There are two main forms of skin cancer: melanoma and nonmelanoma (basal cell carcinoma and squamous cell carcinoma of the skin).
Melanoma is a rare form of skin cancer. Even though melanoma is rare, it is the most common skin cancer in children. It occurs more often in adolescents aged 15 to 19 years. Melanoma is more likely to invade nearby tissues and spread to other parts of the body than other types of skin cancer. When melanoma starts in the skin, it is called cutaneous melanoma. Melanoma may also occur in mucous membranes (thin, moist layers of tissue that cover surfaces such as the lips) and the eye (intraocular melanoma). This PDQ summary is about cutaneous (skin) melanoma. (See the PDQ summary on Childhood Intraocular (Uveal) Melanoma Treatment for more information about intraocular melanoma).
Two other types of skin cancer are basal cell carcinoma and squamous cell carcinoma. They rarely spread to other parts of the body. (See the PDQ summary on Childhood Basal Cell Carcinoma and Squamous Cell Carcinoma of the Skin Treatment for more information on basal cell and squamous cell skin cancer.)
Unusual moles, exposure to sunlight, and health history can affect the risk of melanoma.
Anything that increases your risk of getting a disease is called a risk factor. Having a risk factor does not mean that you will get cancer; not having risk factors doesn't mean that you will not get cancer. Talk with your child's doctor if you think your child may be at risk.
Risk factors for childhood melanoma include the following:
- Having one of the following conditions:
- Giant melanocytic nevi (large black spots, which may cover the trunk and thigh).
- Neurocutaneous melanosis (congenital melanocytic nevi in the skin and the brain).
- Xeroderma pigmentosum.
- Hereditary retinoblastoma.
- A weakened immune system.
- Having a fair complexion, which includes the following:
- Fair skin that freckles and burns easily, does not tan, or tans poorly.
- Blue or green or other light-colored eyes.
- Red or blond hair.
Being White or having a fair complexion increases the risk of melanoma, but anyone can have melanoma, including people with dark skin.
- Being exposed to natural sunlight or artificial sunlight (such as from tanning beds).
- Having several large or many small moles.
- Having a family history or personal history of unusual moles (atypical nevus syndrome).
- Having a family history of melanoma.
Signs of melanoma include a change in the way a mole or pigmented area looks.
These and other signs and symptoms may be caused by melanoma or by other conditions.
Check with your child's doctor if your child has any of the following:
- A mole that:
- changes in size, shape, or color.
- has irregular edges or borders.
- is more than one color.
- is asymmetrical (if the mole is divided in half, the 2 halves are different in size or shape).
- itches.
- oozes, bleeds, or is ulcerated (a condition in which the top layer of skin breaks down and the tissue below shows through).
- A change in pigmented (colored) skin.
- Satellite moles (new moles that grow near an existing mole).
Tests that examine the skin are used to diagnose melanoma.
If a mole or pigmented area of the skin changes or looks abnormal, the following tests and procedures can help find and diagnose melanoma:
- Physical exam and health history: An exam of the body to check general signs of health, including checking for signs of disease, such as lumps or anything else that seems unusual. A history of the patient's health habits and past illnesses and treatments will also be taken.
- Skin exam: A doctor or nurse checks the skin for moles, birthmarks, or other pigmented areas that look abnormal in color, size, shape, or texture.
- Biopsy: A procedure to remove the abnormal tissue and a small amount of normal tissue around it. A pathologist looks at the tissue under a microscope to check for cancer cells. It can be hard to tell the difference between a colored mole and an early melanoma lesion. Patients may want to have the sample of tissue checked by a second pathologist. If the abnormal mole or lesion is cancer, the sample of tissue may also be tested for certain gene changes.
There are four main types of skin biopsies:
- Shave biopsy: A sterile razor blade is used to "shave-off" the abnormal-looking growth.
- Punch biopsy: A special instrument called a punch or a trephine is used to remove a circle of tissue from the abnormal-looking growth.
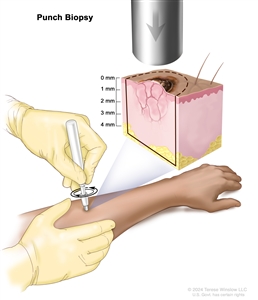
Punch biopsy. A sharp, hollow, circular instrument is used to remove a small, round piece of tissue from a lesion on the skin. The instrument is turned clockwise and counterclockwise to cut about 4 millimeters (mm) down to the layer of fatty tissue below the skin and remove the sample of tissue. Skin thickness is different on different parts of the body. - Incisional biopsy: A scalpel is used to remove part of a growth.
- Excisional biopsy: A scalpel is used to remove the entire growth.



