Respiratory syncytial virus (RSV) causes up to 80,000 hospitalizations and 300 deaths in children under age 5 every year, according to the U.S. Centers for Disease Control and Prevention (CDC). New research confirms the safety of giving ABRYSVO®, an RSV vaccine for adults approved by the FDA for use during pregnancy, to mothers at 32-to-36 weeks gestation to provide much-needed passive immunity and reduce their newborns' risk of RSV. The CDC's Advisory Committee on Immunization Practices recommended the vaccine for eligible pregnant women for the first time last year and are again recommending the vaccine for eligible pregnant women this upcoming RSV season, which starts in September.
NewYork-Presbyterian and Weill Cornell Medicine physicians and scientists, led by maternal-fetal medicine specialist Moeun Son, MD, recently published results from a study evaluating the real-world prenatal use of ABRYSVO® during the 2023-2024 RSV season, and confirmed the findings that there is no increased risk of preterm birth or other adverse perinatal outcomes. Below, Dr. Son describes the study and the implications this has for obstetric care.
Research Goals
RSV is the most common respiratory illness in young children, particularly young infants, and the leading cause of respiratory virus-related hospitalizations for infants in the United States. When nirsevimab, an RSV vaccine for infants, was approved by the FDA last year, access to it was limited to only neonates who were considered high-risk due to a shortage of medication. This ultimately increased the importance of a vaccine that could be given to expectant mothers to reduce their newborn’s risk of getting extremely sick from the respiratory illness.
The initial clinical trial of ABRYSVO® focused on efficacy but also showed a numerical although not statistically significant difference in preterm birth between vaccinated and unvaccinated patients. This raised concerns as people tend to have some hesitancy when there is a new vaccine approved for use during pregnancy. Therefore we wanted to conduct a study in the real-world setting to see if there were any differences in pregnancy outcomes, including those in the initial trial, as well as other important outcomes such as stillbirth, birthweight, neonatal intensive care unit (NICU) admissions, and maternal hypertension.
Research Methods
We analyzed pregnancy outcomes in 1,026 vaccinated and 1,947 unvaccinated patients who received care at NewYork-Presbyterian Weill Cornell Medical Center and Lower Manhattan Hospital during the first year the vaccine was available. Our retrospective observational cohort study included patients who had singleton births at 32 weeks' gestation or later from September 22, 2023, to January 31, 2024. Information about prenatal vaccination with ABRYSVO® was captured from electronic health records.
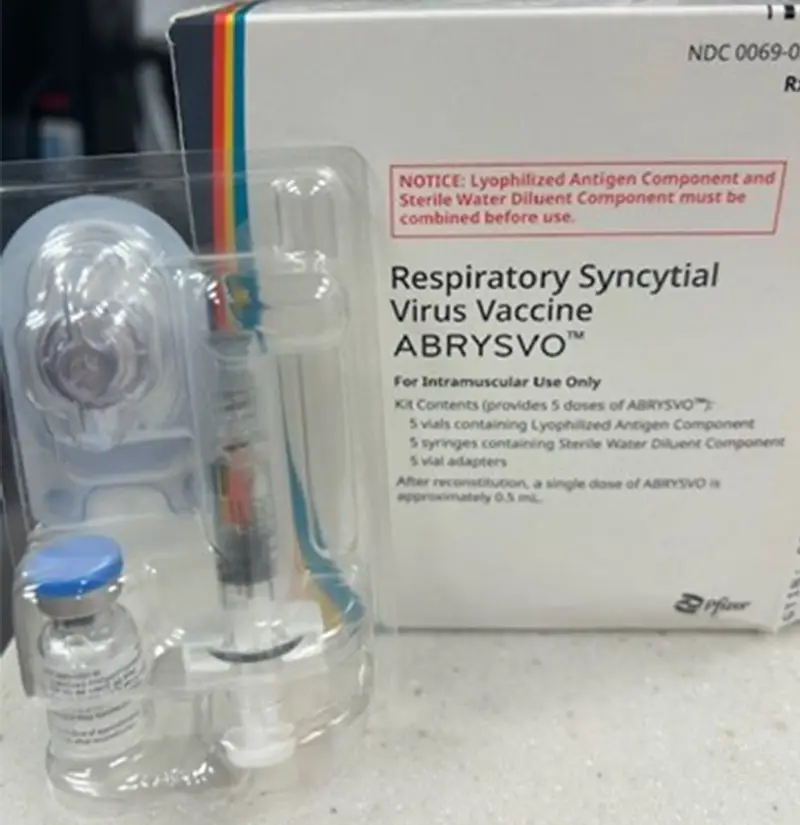
The ABRYSVO respiratory syncytial virus vaccine will be available for administration at most NYP affiliated prenatal offices on September 9, 2024
Key Findings
We were able to vaccinate 35% of the pregnant women under our care — nearly double the national average of 18%. The rate of premature birth was 5.9% among vaccinated women and 6.7% among unvaccinated women, which was not a statistically significant difference. The two groups also had similar rates of stillbirth, small-for-gestational age birthweight, NICU admissions, jaundice, low blood sugar, and sepsis in the newborns.
To verify our results, we conducted three analyses using different statistical methods. In one of those analyses, we found a slightly increased risk of hypertensive disorders of pregnancy in the vaccinated group. Hypertensive disorders of pregnancy range from mild gestational hypertension that happens at term to severe preeclampsia. Most of the cases of hypertension we've seen are mild cases happening at term, but more rigorous studies need to be done to evaluate this association.
Future Implications
This real-world data adds another layer of confidence that the RSV vaccine is safe to administer in pregnant individuals. It is particularly reassuring because it includes women with health conditions that could increase the risk of poor pregnancy outcomes — women who were excluded from the initial efficacy trial.
We are especially proud of our rate of vaccine administration and our ability to quickly make the vaccine available onsite at all our prenatal clinics. At the same time, we identified some disparities in vaccination rates. Black women, those with public insurance, and those who had fewer prenatal visits were less likely to be vaccinated.
As we prepare for the upcoming RSV vaccination season in September, we'll be speaking with the different communities we serve to help us understand what might cause vaccine hesitancy among women or create barriers to access. We want to ensure that all who would benefit will receive the vaccine, with the ultimate goal of a 100% rate of administration.