Oliver Chow, MD, a thoracic surgeon at NewYork-Presbyterian/
Last summer, Dr. Chow successfully treated Arlene Packles, a 73-year-old patient with TBM who had been dealing with a violent, intractable cough for over two years. Below, Dr. Chow discusses TBM, Arlene’s unique case, and how her comprehensive treatment not only cured her debilitating cough, but also gave Packles the best chance for a durable recovery and improved overall quality of life.
What is tracheobronchomalacia (TBM)?
Tracheobronchomalacia (TBM) is a rare disorder caused by the weakening of the cartilage in the trachea and bronchi that typically give airways their proper shape. The weakening causes the trachea and bronchi to lose their structural integrity and for the airway to literally collapse in on itself during expiration, causing TBM to develop. The main symptoms of TBM are a violent cough, which can often sound like barking, dyspnea, and recurrent lung infections.
Ten years ago, TBM was a disease that very few people had even heard about, and surgical interventions offered for this pathology were either quite morbid, or life-altering. A common last resort offered at that time for these patients was a tracheostomy, performed through an opening in the trachea from outside of the neck. Over the past decade, we are understanding more about TBM and have developed an innovative surgical approach, robot-assisted tracheobronchoplasty, to reconstruct and provide renewed structure to the central airways.
What symptoms was Arlene experiencing and how did she come to receive a TBM diagnosis?
For over two years, Arlene experienced a progressive and refractory cough, along with dyspnea. She saw several doctors, including her primary care physician and an otolaryngologist, but they were stumped as to what was causing her issues. Eventually, she was referred to my colleague Dr. Shostak, who, after learning more about her symptoms, performed a dynamic bronchoscopy. During that procedure, he found that Arlene had a severe degree of collapse in her airway – when she was exhaling, her airway collapsed nearly 100%. Essentially, every time she was breathing out, the entire back of her airway was collapsing in on itself. After seeing that, Dr. Shostak diagnosed her with severe TBM and referred her to me for surgical treatment.
Why did it take so long for Arlene to get an accurate diagnosis?
TBM is an extremely underrecognized disease and hard to detect unless you are looking for it. The main symptoms – cough, dyspnea, and recurrent lung infections – show up in many other pathologies. Although a lot more has been learned about the disease in the past decade, many first line providers who see patients with these symptoms still don’t know much about TBM.
Many patients will be diagnosed with other conditions, such as chronic obstructive pulmonary disease (COPD), asthma, viral infections, ENT issues, and vocal cord dysfunction, when the actual diagnosis is TBM. Sometimes these other conditions do coexist with TBM and it’s common for us to hear stories of individuals being diagnosed with one of these diseases and receiving some sort of intervention. The patient will get marginally better, but there won’t be a significant change in their symptomology. Ultimately, they will eventually be seen by someone who is familiar with TBM and then refers them to a center like ours that has extensive expertise in this pathology. This was true in Arlene’s case.
What risk factors did Arlene have that led to her developing TBM?
There are a handful of risk factors associated with the development of TBM, which range from underlying genetic conditions, such as Ehlers-Danlos syndrome, birth defects, trauma, inflammatory conditions, and others. In adults, TBM is almost always associated with other medical conditions and in Arlene’s case, she had longstanding, silent gastroesophageal reflux disease (GERD) and obesity, both of which were interfering with her breathing. Our team determined that stomach acid had been spilling into her airways for several years, causing chronic inflammation and the deterioration of the supportive airway structures, which ultimately led to the collapse of her trachea and bronchi.
How did you decide on the treatment plan for Arlene, and what did her treatment entail?
To devise an appropriate treatment plan for Arlene, we needed to determine the optimal sequence of procedures. This is done in concert with the patient to determine the severity of symptoms and to what degree they are affecting their health and quality of life.
For Arlene, we had to decide whether to address the TBM, reflux, or obesity first. Research has shown that in patients with severe TBM and reflux, treating the reflux first results in better overall outcomes. However, when Dr. Shostak and I met with Arlene and her husband, she expressed that because her symptoms were so severe, she didn’t want to undergo any other treatments first because she felt the cough and breathing were so hindering to her. So ultimately we decided to treat her by performing a minimally invasive robot-assisted tracheobronchoplasty.
I performed Arlene’s surgery by making five small incisions and suturing a synthetic mesh to the outside of the trachea and mainstem bronchi, stenting them to their proper position and preventing the posterior membrane of the airways to protrude and collapse in on itself. With its magnified 3D views, interactive platform and wristed instrumentation, the robotic approach enables me to perform a precise dissection and restoration of the airway.
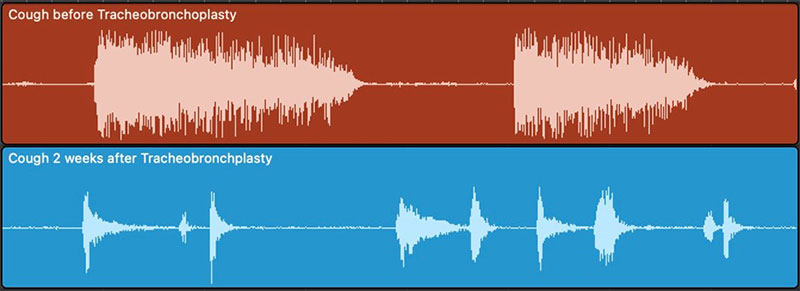
Visual waveform representation of this patient’s cough before (red, above) and after (blue, below) surgical tracheobronchoplasty.
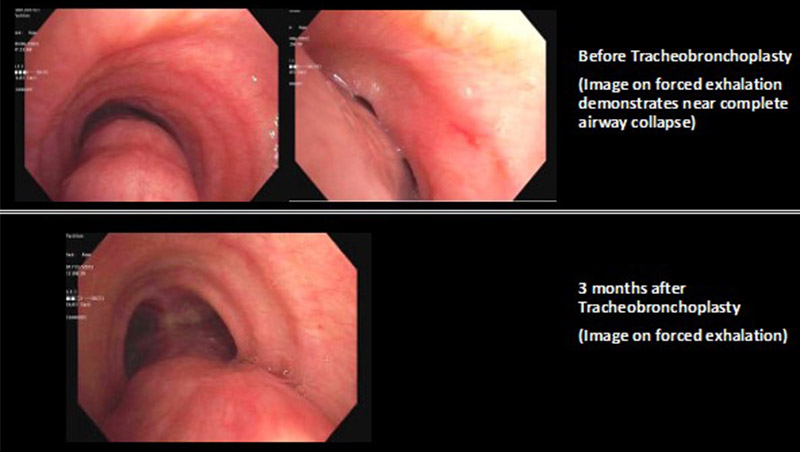
Dynamic bronchoscopy demonstrating improved structure and decreased airway collapse on exhalation after surgical tracheobronchoplasty.
The day after her surgery, Arlene’s cough had already improved markedly. She left the hospital four days after the operation. The violent cough that had plagued her for several years was gone.
It’s been over a year since Arlene had her tracheobronchoplasty – how is she doing now?
Arlene’s main symptom of cough was improved dramatically by the surgery. Arlene initially had not planned on having bariatric surgery; however, the tracheobronchoplasty enabled her to regain sufficient strength to withstand subsequent procedures, which would provide long-term benefits. In March 2023, Kartik Sampath, MD, performed a transoral incisionless fundoplication to address her reflux and an endoscopic sleeve gastroplasty, which reduced her stomach's size by about 70 percent. She is doing extremely well now and enjoying her life again.
What enables you to excel in the treatment of TBM?
We are one of several places in the country that have a program dedicated to this rare disease. Our program offers a true multidisciplinary approach to diagnosing and treating the condition that involves pulmonology, laryngology, bariatrics, gastroenterology, and thoracic surgery. Few other centers have specialists with such a wide range of expertise in the pathologies associated with TBM. We work together to review each individual case with the overarching goal of helping patients breathe naturally and effectively by addressing their symptoms.