For adolescents and young adults (AYA) with cancer, reproductive health is a key concern that is often addressed through discussions around fertility preservation prior to starting treatment. However, AYA cancer survivors often have little knowledge of how their fertility or reproductive goals can be impacted post-treatment by the therapies they underwent or their cancer-related comorbidities.
To help physicians educate their patients on this topic both before and after treatment, James A. Kashanian, MD, Director of Male Sexual Health in the Department of Urology at NewYork-Presbyterian and Weill Cornell Medicine, along with his colleagues at The Oncofertility Consortium, recently published a comprehensive review articlein Pediatric Blood & Cancer as part of their special series on fertility considerations in survivorship. “The information provided is particularly helpful for clinicians seeking to incorporate fertility services in their survivorship clinic, or to help guide patients inquiring about fertility concerns in their decision-making,” says Dr. Kashanian.
Below, Dr. Kashanian highlights some of the goals and guidelines discussed in the paper, and what physicians treating AYA cancer patients need to know.
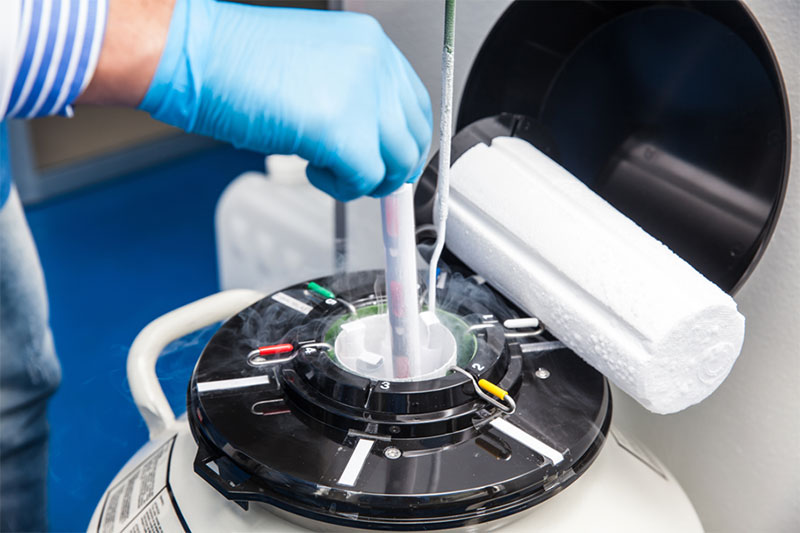
Liquid nitrogen cryogenic tank at life sciences laboratory
How knowledgeable are physicians and patients generally about reproductive health for AYA cancer patients?
It has gotten much better over the past decade or so, but there are still gaps. Ten years ago, during my fellowship at Northwestern University, I was one of the authors on an article that highlighted the lack of comfort and formal education that many pediatric oncology healthcare providers had on the topic of fertility preservation. The article brought this issue to the forefront and now most, if not all, oncology fellowships offer specific curriculums that focus on fertility preservation. The resources now available to patients, their families, and healthcare providers on those options are vast and comprehensive. But young cancer survivors still demonstrate little understanding of their infertility risk and uncertainty over their fertility status. It is our job as physicians to make sure they are educated about all the ways their treatment may impact their future fertility.
What are some of the common misconceptions about fertility that you’re trying to combat?
Patients often over- or underestimate their treatment-related fertility risks. In my experience, male patients often don’t realize that they have multiple options for fertility preservation and that sperm can remain cryopreserved for decades prior to use. They may believe that a normal testosterone level and normal sexual function equates to fertility. Because spermatogenesis is much more sensitive to damage than the Leydig cells that make testosterone, males can have normal testosterone levels, normal virilization, and normal sexual function but be oligospermic (have low sperm count) or azoospermic (no sperm count).
For female patients, they may assume that if they are not having regular periods or any periods at all, then they cannot become pregnant. This makes it important for physicians to emphasize that pregnancy can still occur and contraception should be used. Conversely, if some patients are having periods, they expect that they will be able to become pregnant in the future. Despite having menses, they can still experience decreased ovarian reserve and primary ovarian insufficiency, potentially preventing a pregnancy.
What are some of the biggest fertility considerations for AYA male patients?
My main concern for adolescent males is whether spermatogenesis and spermarche have begun. If the process has not begun, there are research protocols that allow for testicular biopsies to be taken and for spermatogonial stem cells to be cryopreserved. Although experimental, the hope is that these spermatogonial stem cells can one day be matured in vivo or in vitro to sperm for future use with assisted reproductive techniques such as intracytoplasmic sperm injection for in vitro fertilization. However, the maturation of spermatogonial cells is not possible at this time.
In male AYA patients who can give a semen sample, cryopreservation of ejaculated sperm is the easiest and most effective way to preserve fertility prior to receiving gonadotoxic treatment. Oftentimes, it may be as easy as a semen analysis. When an ejaculated sample cannot be supplied because, for example, the patient is azoospermic or too ill, or for religious reasons, we can perform interventional procedures to retrieve sperm via electroejaculation. Surgery can also be performed to retrieve sperm from the testicle. In cases of non-obstructive azoospermia, microdissection testicular sperm extraction remains the gold standard.
Conversely, what are the key considerations for female patients?
Many studies indicate that female AYA cancer patients are less likely to be offered counseling or be referred to fertility preservation centers than their male counterparts. They may therefore have an even bigger lack of understanding about how cancer treatment impacts fertility and options for fertility preservation procedures.
Ovarian function is key to fertility in female AYA survivors and can be evaluated with serum hormone levels and ultrasonography. However, traditional measures of ovarian function, follicle-stimulating hormone, and estradiol may not reflect the extent of damage to the primordial follicle pool and the decrease in ovarian reserve following cancer treatment.
That’s why it’s important to discuss the level of risk for ovarian dysfunction related to cancer treatment therapy prior to starting treatment, as it may guide counseling and help identify patients who need careful monitoring.
What is one overarching takeaway you have for physicians treating AYA cancer patients?
In our article, we present approaches to counseling AYA about fertility and the factors to consider to help you determine the content and timing of those discussions. Importantly, fertility is an issue to address in survivorship even if infertility risk and preservation options were already discussed at diagnosis.
Prior to beginning treatment, I also advocate for AYA patients to have multidisciplinary care teams of oncologists, endocrinologists, psychologists, and reproductive medicine specialists so that they have the most optimal reproductive health and fertility guidance. This is an approach we take at NewYork-Presbyterian and Weill Cornell Medicine. Our cross-collaborative efforts among pediatrics, pediatric and adult oncology, endocrinology, and pediatric genetics helps us to identify patients with the highest risk of future infertility and guide them on the right path early on for fertility preservation treatment.




