
Stephanie Lovinsky-Desir, MD, MS
Children living in urban neighborhoods are at a disproportionate risk of developing asthma, one of the most common chronic diseases in children. While exposure to air pollutants has long been associated with increased risk for asthma, few studies have explored the molecular mechanisms by which air pollution triggers an asthma attack. To bridge this knowledge gap, Stephanie Lovinsky-Desir, MD, MS, Chief of the Pediatric Pulmonary Division at NewYork-Presbyterian/Columbia, Meyer Kattan, MD, Director of the Pediatric Pulmonary Division at NewYork-Presbyterian/Columbia, and other members of the Childhood Asthma in Urban Settings (CAUSE) network, conducted a retrospective analysis to explore the association between regional air pollution and respiratory outcomes in children and adolescents with asthma, particularly asthma exacerbations occurring in the absence of respiratory virus. The findings may lead to effective treatment and prevention approaches tailored to children in urban communities.
Children who were exposed to high concentrations of air pollutants and did not have a respiratory virus present were significantly more likely to have asthma attacks.
— Dr. Stephanie Lovinsky-Desir
“We know that increased exposure to air pollutants is associated with a greater risk of asthma and prevents healthy lung development in children,” explains Dr. Lovinsky-Desir. “Our studies within the CAUSE network seek to understand the reasons why children living in urban communities have more asthma and worse asthma outcomes compared to children living in other types of communities. The study findings will go a long way toward bringing effective therapies to this group of individuals who otherwise would not have access to cutting edge asthma therapies.”
During an asthma attack, the lining of the airway swells, muscles around the airways contract, and the airways produce extra mucus, which narrows the space for air to move in and out of the lungs. Although respiratory viral infections are a common cause of asthma in children, other non-viral agents, including bacterial infections, allergens, pollen, and air pollutants, can also trigger asthma attacks.
This retrospective analysis is one of the latest initiatives of the CAUSE network, a research consortium funded by the National Institute of Allergy and Infectious Diseases (NIAID), to better understand and reduce the disproportionate burden of asthma among children living in low-income urban environments.
“The main objective of the study was to investigate the associations between regional air pollution and respiratory outcomes in children with asthma, particularly asthma exacerbations occurring in the absence of respiratory virus,” says Dr. Lovinsky-Desir. “An additional objective of this study was to investigate the molecular mechanisms by which air pollution triggers asthma exacerbations.”
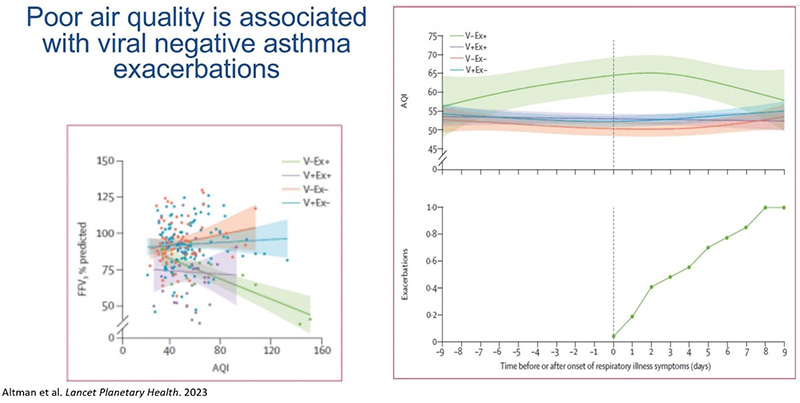
(L) Associations of pulmonary functions with AQI values; (R) AQI values and onset of respiratory symptoms among children with and without viral induced exacerbation
In the study, the researchers investigated the associations between air pollutant concentrations, respiratory illnesses, lung function, and upper airway transcriptional signatures in children with asthma living in urban locations, with particular focus on asthma exacerbations occurring in non- respiratory viral infections. The team performed a retrospective analysis of data from the MUPPITS1 (Mechanisms Underlying Asthma Exacerbations Prevented and Persistent with Immune-Based Therapy) cohort and validated their findings in the ICATA (Inner-City Anti-IgE Therapy for Asthma) cohort. The researchers included participants from the MUPPITS1 cohort who reported a respiratory illness at some point during the follow-up visits and participants from the ICATA cohort who had nasal samples collected during respiratory illness or at a scheduled visit. The team used Air Quality Index (AQI) values and air pollutant concentrations for particulate matter, ozone, nitrogen dioxide, sulfur dioxide, carbon oxide, and lead from the U.S. Environmental Protection Agency (EPA) spanning the years of both cohorts, and matched values and concentrations to each illness for each participant. The researchers investigated the associations between regional air pollutant concentrations and respiratory illnesses and asthma exacerbations, pulmonary function, and upper airway transcriptional signatures.
Both cumulative Air Quality Index values and individual pollutants were associated with altered gene expression in inflammatory pathways, mucus secretion and airway remodeling that occur during an asthma exacerbation.
— Dr. Stephanie Lovinsky-Desir
The researchers found that increased levels of two outdoor air pollutants—ozone and fine particulate matter— were significantly associated with asthma exacerbations and decreases in pulmonary function in the absence of a provoking viral infection. “The main finding was that high concentrations of air pollutants among children who did not have a respiratory virus present was significantly associated with having asthma attacks,” says Dr. Lovinsky-Desir. “The study also found that both cumulative AQI values and individual pollutants were associated with altered gene expression in inflammatory pathways, mucus secretions and airway remodeling that occur during an asthma exacerbation.”
The AQI is readily available to patients and helps to translate what we’re seeing in the study to actual clinical practice. We can all keep track of air quality on a daily basis, and we can teach our patients to keep track of air quality, particularly if they have asthma.
— Dr. Stephanie Lovinsky-Desir
One key benefit of the study is its use of the AQI, a publicly available tool, to identify poor air quality. “The AQI is readily available to patients and helps to translate what we’re seeing in the study to actual clinical practice,” she says. “We can all keep track of air quality on a daily basis, and we can teach our patients to keep track of air quality, particularly if they have asthma.”
“The AQI levels that were observed in this study were actually below the level that usually triggers a warning as being unsafe for sensitive populations like the elderly and those with asthma,” notes Dr. Lovinsky-Desir, who sat on the EPA’s Clean Air Scientific Advisory Committee. “We are seeing effects of air pollution at relatively lower levels, which indicates that the EPA needs to lower the thresholds for what is safe and acceptable air quality levels for particulate matter and ozone.”
The CAUSE network is also conducting clinical studies of new biologic medications for the treatment of moderate-to-severe asthma. Made from the cells of a living organism, such as bacteria or mice, biologics are modified to target specific antibodies, inflammatory molecules or cell receptors in humans to disrupt the pathways that lead to asthma exacerbations.
“These studies have a common end goal, which is to ensure that children in our communities can breathe well and live active, healthy lives,” says Dr. Lovinsky-Desir. “I look forward to participating in future research initiatives that bring us closer to this goal.”




