Joseph Picoraro, MD, a pediatric gastroenterologist at NewYork-Presbyterian and Columbia, has been motivated to find the least invasive ways to treat strictures, or a narrowing in the intestines, that many of his pediatric patients with inflammatory bowel disease (IBD) and other digestive conditions often experience. He is a leader in the use of endoscopic electroincision therapy (EIT) and was trained in this procedure under the guidance of Bo Shen, MD, Director of the IBD Center and Co-director of the Global Center for Integrated Colorectal Surgery and IBD Interventional Endoscopy at NewYork-Presbyterian and Columbia.
EIT is an alternative interventional method that can be used to treat strictures and preserve the bowel, and Dr. Picoraro is only one of several pediatric gastroenterologists nationwide who is performing this procedure to help patients. He discusses how this novel endoscopic approach works and how NewYork-Presbyterian and Columbia are advancing the use of it to improve patient care.
What is endoscopic electroincision therapy and how is it performed?
As gastroenterologists, we’re trained to perform endoscopy to diagnose a variety of digestive conditions, like IBD, as well as other procedures such as endoscopic balloon dilation (EBD). Endoscopic electroincision therapy (EIT) builds off our use of endoscopy and applies it in a new, minimally invasive way to treat strictures.
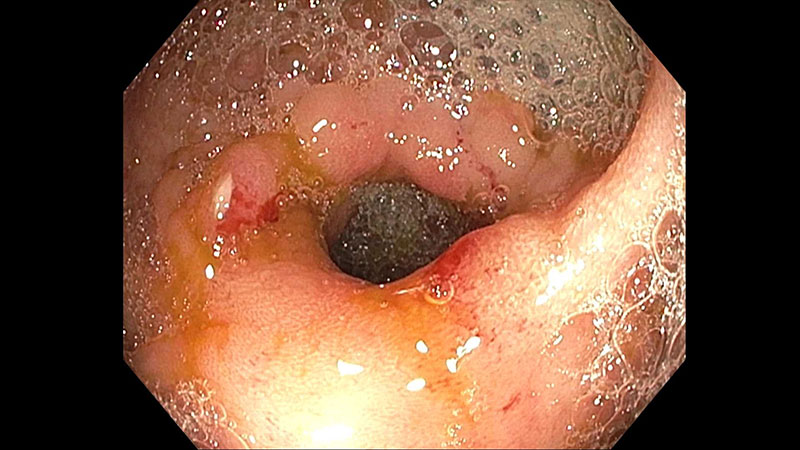
Intestinal stenosis as seen during endoscopy
During EIT with stricturotomy and/or strictureplasty, we insert an endoscope rectally into the patient and guide it up to where the narrowing is. We then utilize small tools to cut away at the fibrotic tissue to make the intestinal opening larger (stricturotomy) and place endoscopic clips (strictureplasty) to make the cut more durable.
What made you interested in EIT as a treatment modality?
EIT is really in its infancy as a field, and even more so in the treatment of children, but there are a lot of potential benefits from this approach. In EIT, we control exactly where we cut, allowing us to be more precise and target the stricture at its exact location. EIT appeals to me because it is an effective treatment for their stricture with more accuracy and it helps preserve their bowel, all while using a non-surgical approach.
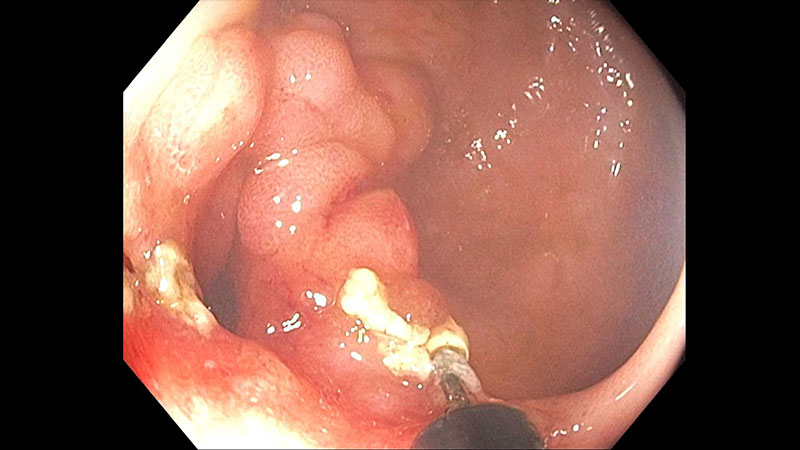
Utilizing EIT to perform a stricturotomy
When Dr. Shen arrived at NewYork-Presbyterian and Columbia in 2019, I was immediately drawn to the work he was doing using EIT and other endoscopic approaches in adults and began training and collaborating with him on cases. Last year, I received funding from the North American Society of Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN), to complete a formal training fellowship with Dr. Shen, and now I am one of a few pediatric gastroenterologists in the country who is able to perform stricturotomy and strictureplasty with EIT.
What are the benefits and/or potential challenges of the available treatments for strictures?
Traditionally, treatment of a stricture has been either via EBD or surgery. EBD uses pressure to open the narrowing in the general location of the stricture. The challenge with EBD is that you can’t control the exact location where the tear in the tissue occurs to open the stricture, and there are risks of perforation or incisions occurring in locations that lead to the development of fistulae.
If a patient isn’t a candidate for EBD, then they are typically referred to a surgeon to have a surgical strictureplasty or bowel resection. Surgery comes with its own inherent risks, particularly for children, and repeat surgeries may be required in the future if the stricture develops at the anastomosis or another location, which means losing more bowel. The more bowel that is surgically removed, the more at-risk children become for developing short bowel syndrome, growth issues, and other complications.
What factors make a patient a good candidate for EIT?
It’s dependent on each individual case but generally, a candidate for stricturotomy and/or strictureplasty with EIT is someone with IBD who has irreversible bowel damage where surgery would be the next step. Ideally, we’d also like them to have their inflammation under control. Lastly, the best stricture for endoscopic intervention is an anastomotic stricture because we know it’s mostly going to be from fibrotic tissue. Once we decide that a patient is a good candidate, we assess whether the potential benefits outweigh the potential risks. Then it comes down to what we think we can actually achieve endoscopically, some of which evolves during the procedure itself.
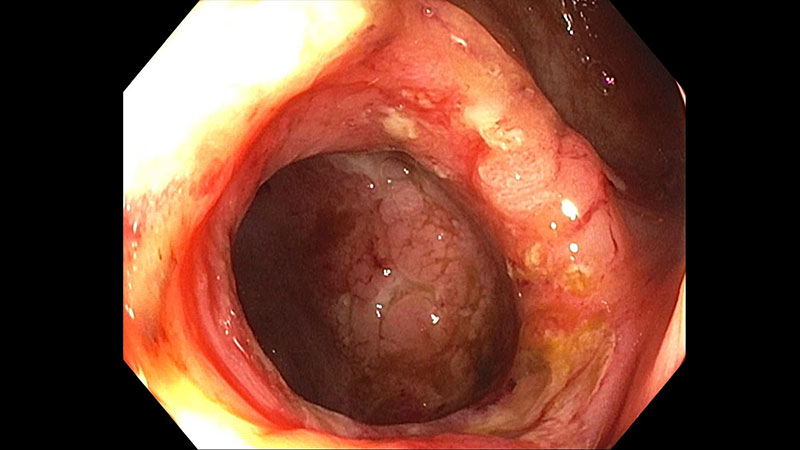
Stricture resolved following EIT
While IBD is one of the main indications for use of this modality, this can also be used in patients with other conditions who develop post-surgical complications in the gastrointestinal tract. I had a patient who was born with necrotizing enterocolitis and had undergone multiple bowel surgeries, leaving them in intestinal failure and dependent on total parenteral nutrition (TPN). They developed another stricture and had undergone several EBDs to open the narrowing, but that wasn’t solving the issue. So, to save their remaining bowel and avoid another surgery, I performed a stricturotomy and strictureplasty with EIT. The procedure went extremely well; they are growing well and haven’t had any further strictures or blockages. Additionally, the patient previously had a lot of feeding intolerance and inability to progress with their feeds. After the procedure, they were able to wean off TPN and no longer needed a central line.
What research are you conducting looking at the use of EIT among pediatric patients?
While this modality is being adopted in adults, use in pediatrics is growing slowly. We recently presented a paper at a conference that showed the outcomes of a retrospective cohort study of 10 pediatric patients, totaling 18 procedures, with anastomotic and primary luminal stricture who underwent EIT with stricturotomy and/or strictureplasty. The results were promising:
- Two patients did not require further intervention and had no stricture recurrence at follow-up.
- Three patients required repeat interventions but could wait longer in between interventions when compared with how frequently they previously had to get EBDs.
- There were no episodes of GI bleeding.
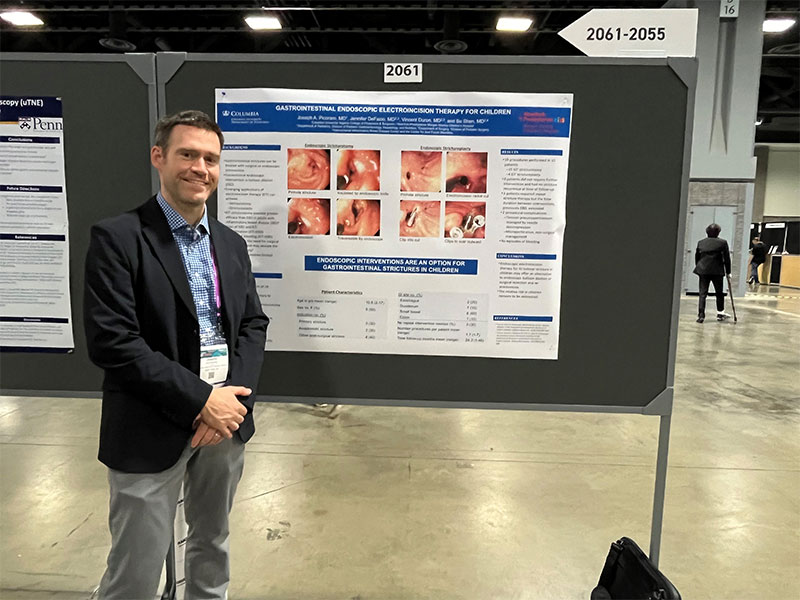
Dr. Picoraro with his poster on gastrointestinal endoscopic electroincision therapy for children.
Although this was a small study, it does demonstrate the potential success that EIT can have in pediatric patients as an alternative to EBD or surgery. We’re continuing to follow the cohort at NewYork-Presbyterian and Columbia to assess the outcomes of EIT among our patients.
What is critical to the success of performing EIT?
If you have a challenging case where a conventional approach is not working and surgery is not desired but is on the table, then we need to think about whether an endoscopic approach would be the right fit for the patient. The decision to perform EIT with stricturotomy and/or strictureplasty needs to be made by a multidisciplinary team of specialists who work closely together to ensure the best outcomes. Additionally, you want to make sure that you perform it at an integrated medical center, like NewYork-Presbyterian and Columbia, that is equipped to handle a variety of conditions and treatment modalities. The multidisciplinary nature of what we provide here is the cornerstone of our care and essential to successfully performing EIT.




