An energetic partnership between NewYork-Presbyterian and Weill Cornell Medicine has propelled the transformative growth of the Department of Ophthalmology at NewYork-Presbyterian/Weill Cornell Medical Center. This growth and expansion is particularly notable in the increased volume and sophistication of its clinical care services, advantaged by New York City’s patient population with its unmatched size, medical complexity, and diversity.
Extraordinary Facilities
NewYork-Presbyterian/Weill Cornell now contains three of the world’s most sophisticated operating rooms for eye surgery at the hospital’s newly constructed NewYork-Presbyterian David H. Koch Center. Within these remarkable operating rooms, our ophthalmic surgeons utilize the latest technologies to achieve exceptional precision in the restoration of vision from many common disorders, such as cataract, corneal and retinal diseases, glaucoma, and many more.
The Department has experienced unprecedented growth in surgical volume with the opening of this facility. In the first year of operation, the number of surgical procedures grew 34 percent, and in the subsequent months, volume increased by an additional 21 percent. Detailed attention to patient flow and every element of the patient experience has resulted in exceptionally positive satisfaction ratings, and the greatly improved operational efficiencies have enabled the Department to perform over 3,900 ophthalmic surgeries per year. The NewYork-Presbyterian David H. Koch Center is particularly comforting to children, and patients of Richard L. Levy, MD, Director of Pediatric Ophthalmology, “drive” to the operating room in tiny sports cars alongside their parents.

The NewYork-Presbyterian David H. Koch Center features three state-of-the-art ophthalmic operating rooms.



The Department of Ophthalmology at Weill Cornell has constructed new office suites off-site to accommodate its growth and expansion.
Space is always a challenge in Manhattan, and the Department’s growth to 33 providers and 85,000 patient visits at the main medical center on the Upper East Side requires continued development of new office suites. The Department has opened its most recent satellite in TriBeCa to accommodate the rapidly growing population in Lower Manhattan. This state-of-the-art, 8,000-square-foot facility Postoperative image following DMEK, which preserves normal corneal anatomy The NeuroOphthalmology Service treats complex conditions that affect vision and eye movements. Keratoprosthesis surgery provides a viable option to corneal transplantation. hosts the full range of ophthalmic subspecialties and has become so popular that it exceeded projections in the first year of operation. With the addition of NewYork-Presbyterian Brooklyn Methodist Hospital as part of the NewYork-Presbyterian enterprise, a similar outpatient office is planned for Brooklyn, and a new eye operating room is nearly completed at that hospital.
Transforming Ophthalmic Surgery
Permanent Keratoprosthesis
Kimberly C. Sippel, MD, Director of the Cornea and Anterior Segment Service, with her associates Christopher E. Starr, MD, and Ana Alzaga Fernandez, MD, have developed a nationally prominent center for the implantation of permanent keratoprosthesis. Using the Boston/Dohlman device, and operating in conjunction with Donald J. D’Amico, MD, Ophthalmologist-in-Chief at NewYork-Presbyterian/Weill Cornell, and Szilard Kiss, MD, Anton Orlin, MD, and Athanasios Papakostas, MD, members of the Vitreoretinal Service, they have been able to offer this sight-saving procedure to many visually desperate patients for whom conventional types of corneal transplantation are prone to failure.
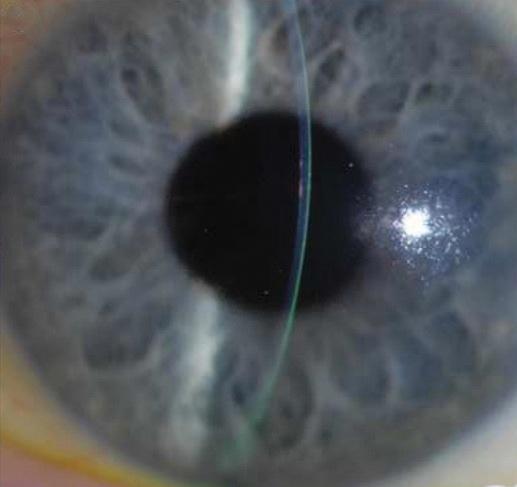
Postoperative image following DMEK, which preserves normal corneal anatomy
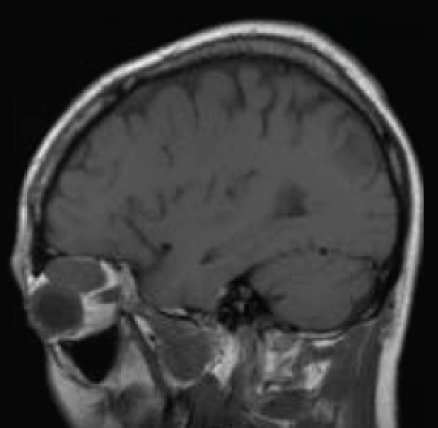
The NeuroOphthalmology Service treats complex conditions that affect vision and eye movements.
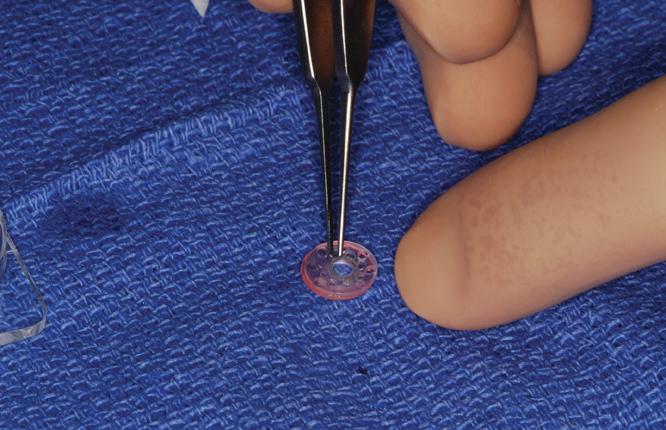
Keratoprosthesis surgery provides a viable option to corneal transplantation.
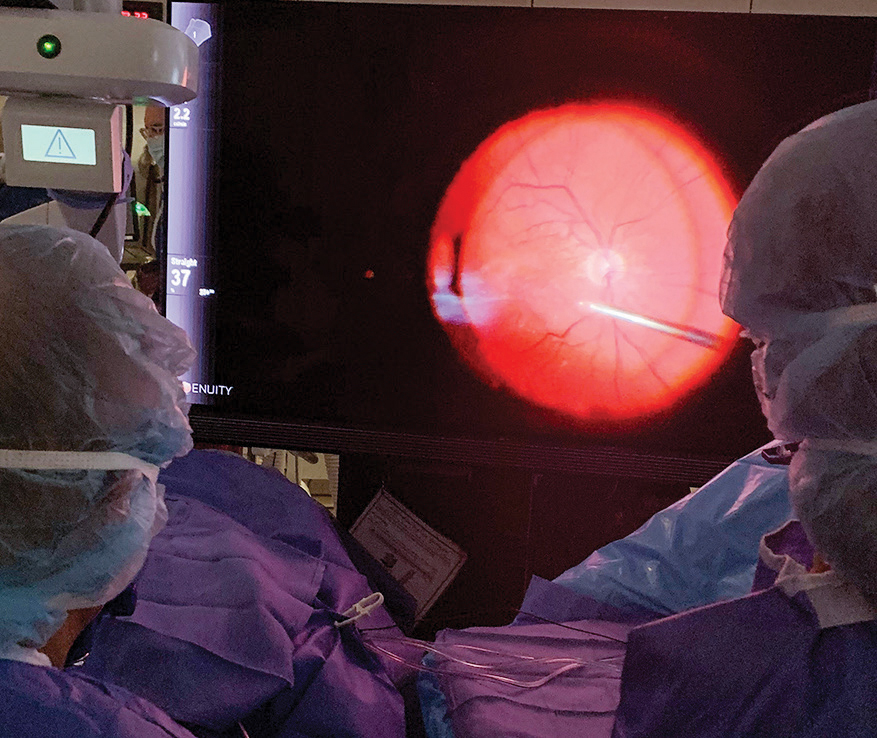
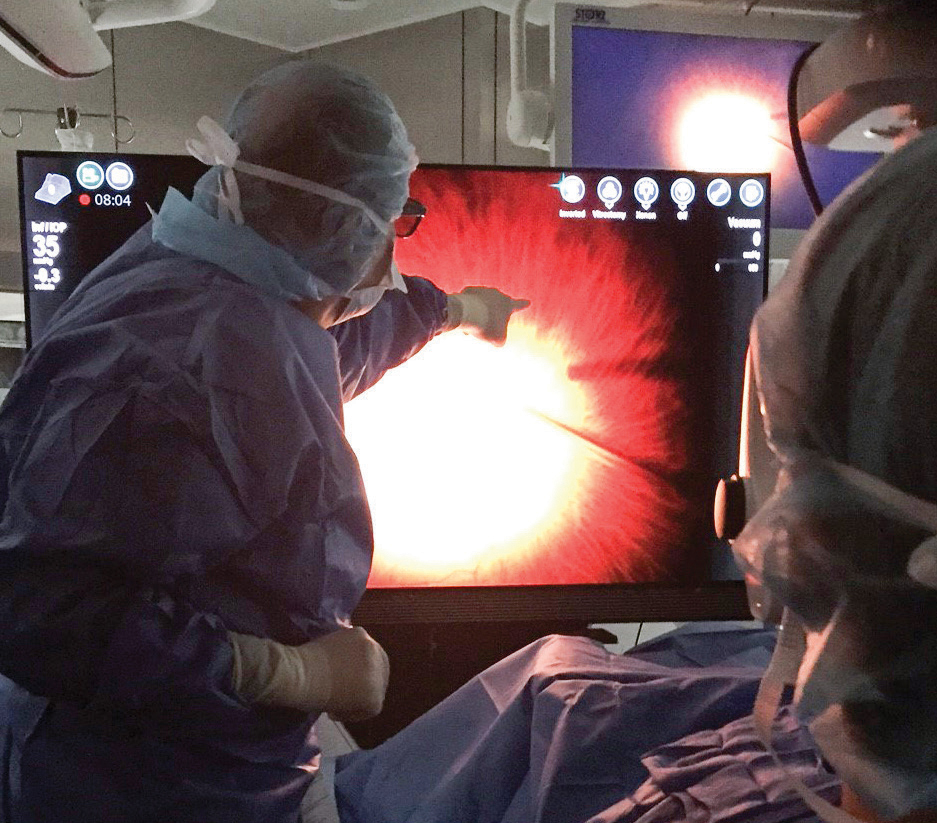

The latest digital visualization system replaces the traditional operating microscope, enabling the surgeon to view the surgical field on a six-foot plasma screen through stereo glasses.
Amniotic Membrane Application
Dr. Sippel and the cornea team pioneered acute application of amniotic membrane for the treatment of severe ocular surface disease in Stevens Johnson Syndrome and related conditions. They continue using this technique to successfully restore vision in patients with no other alternatives. Their approach has been adopted in many burn centers around the country.
Prosthetic Scleral Lens
With Michelle N. Lee, OD, the Department has the largest PROSE lens program in New York. This lens covers the ocular surface completely, and its use allows successful treatment of many complex ocular surface and oculoplastic conditions that present to the Department’s physicians.
Oculoplastics
Led by Gary J. Lelli, Jr., MD, the Oculoplastics Service has become the largest in the city with four attendings – Benjamin Levine, MD, Kira L. Segal, MD, Kyle Godfrey, MD, and Dr. Lelli – and hosts the only ASOPRS approved fellowship in New York City for this elegant and demanding specialty. The growth in complex multidiscipline surgery with Neurological Surgery, ENT, and Dermatology has resulted in exceptionally high demand for Oculoplastics expertise at Weill Cornell. Similar multidisciplinary issues and complexity have fueled the growth of the Neuro-Ophthalmology Service. Led by Marc J. Dinkin, MD, and with Cristiano Oliveira, MD, the service has grown to offer two busy fellowship positions per year.
The growth in complex multidiscipline surgery with Neurological Surgery, ENT, and Dermatology has resulted in exceptionally high demand for Oculoplastics expertise at Weill Cornell.
Weill Cornell ophthalmologists can offer patients the noninvasive femtosecond laser-assisted cataract surgery.
A Focus on Advanced Technology
Ninety percent of vitreoretinal surgeries and an increasing number of anterior segment surgeries in the NewYork-Presbyterian David H. Koch Center are now performed using the latest digital visualization system that replaces the traditional operating microscope, enabling the surgeon to view the surgical field on a six-foot plasma screen through stereo glasses. This system – the first of its kind in New York City – offers tremendous magnification as well as full digital control of illumination. These features greatly increase the surgeon’s depth of field and enhance the ability to perform microscopic manipulations of delicate retinal and other ocular tissues with far greater accuracy and safety.
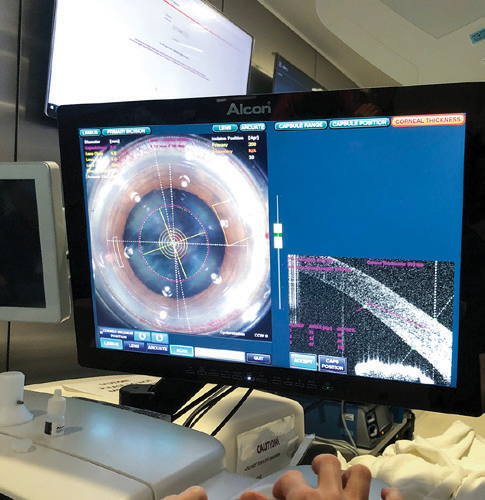
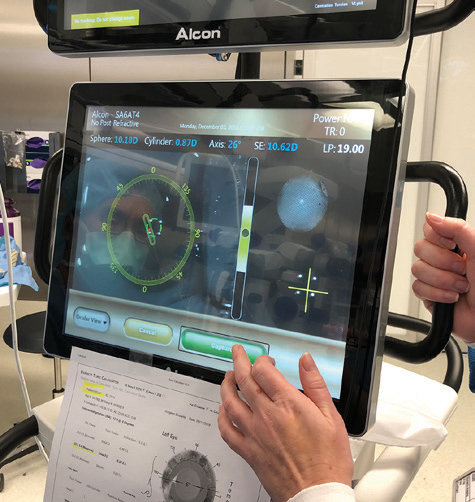
Additional advanced technologies in the NewYork-Presbyterian David H. Koch Center ophthalmic operating rooms include New York’s newest femtosecond laser for cataract extraction, as well as two innovative optical systems for measuring the refractive power of the eye during surgery itself. These revolutionary devices assist in the selection of the optimal custom intraocular lens for a given patient and correct for any surgically induced changes in the final lens selection.
As a result of these advances and capabilities, visual results after cataract extraction by NewYork-Presbyterian/Weill Cornell surgeons have been documented to exceed national averages.
As a result of these advances and capabilities, visual results after cataract extraction by NewYork-Presbyterian/Weill Cornell surgeons – Edward C. Lai, MD, Jessica B. Ciralsky, MD, Ashley Brissette, MD, MSc, Benjamin Levine, MD, Christopher E. Starr, MD, Kimberly C. Sippel, MD, Grace Sun, MD, Ana Alzaga Fernandez, MD, Sirikishan R. Shetty, MD, Sarah Van Tassel, MD, Jeffrey F. McMahon, MD, Leila Rafla-Demetrious, MD, Stephanie Muylaert, MD, Paul Petrakos, DO, MS, Shaily Shah, MD, Anna-Maria Demetriades, MD, PhD, and others – have been documented to exceed national averages. A recent review of all cataract surgeries available in our Epic database documented postoperative visual acuity results of 20/40 or better in 97 percent of patients who did not have pre-existing vision limiting comorbidities, such as macular degeneration, compared to the nationally published average in which 94.6 percent of patients attain such an acuity.


The latest ophthalmic surgical microscopes provide exquisite illumination and magnification.
After decades of limited surgical options, innovation in the surgical treatment of glaucoma has become one of the most exciting growth areas in eye surgery with many new devices and procedures for intraocular pressure control. Co-Directors Stephanie Muylaert, MD, and Sarah Van Tassel, MD, along with Leila Rafla-Demetrious, MD, Anna-Maria Demetriades, MD, PhD, and Paul Petrakos, DO, MS, combine new diagnostic tools, such as daily home pressure monitoring, with the vast surgical armamentarium available within the NewYork-Presbyterian David H. Koch Center to allow increasingly precise and customized treatment.



