Every year the American Gastroenterological Association (AGA) hosts Digestive Disease Week® (DDW), an international gathering of gastroenterology and hepatology experts who care for the 60 million to 70 million Americans affected by digestive diseases, which can range from biliary tract diseases to functional gastrointestinal and motility disorders to liver and pancreatic diseases.
NewYork-Presbyterian clinicians attended and presented at DDW 2024 on a variety of topics across all digestive diseases. Photo credit: Digestive Disease Week®.
Dozens of clinicians from across NewYork-Presbyterian attended and presented at DDW 2024, held in May in Washington, D.C. Below are highlights from some of those presentations.
Prescribing Patterns for Pediatric Patients with Functional Constipation and IBS-C
Functional constipation (FC) and irritable bowel syndrome (IBS) are common childhood conditions accompanied by chronic, burdensome symptoms. Although there are many treatments FDA approved for adults with these conditions, few treatments are approved for use in children.
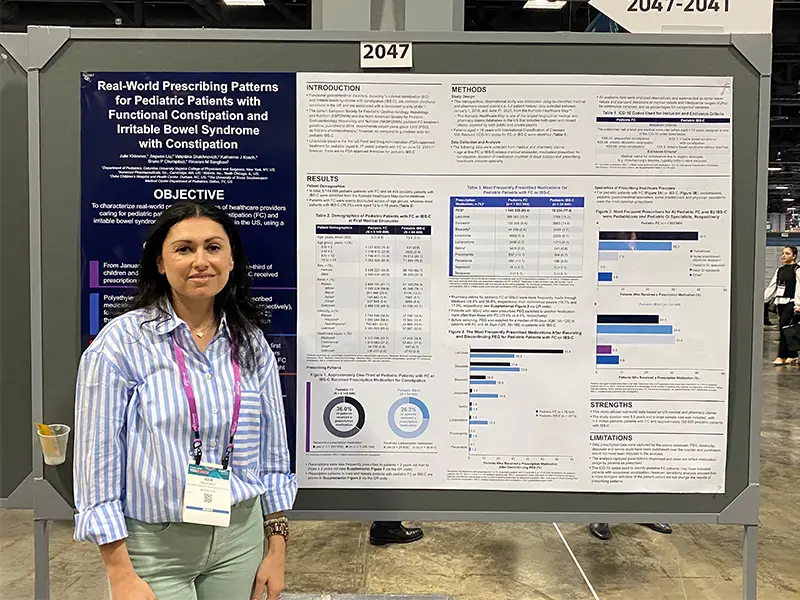
Dr. Khlevner’s research focused on which medications are being prescribed to pediatric patients with FC and IBS-C, despite the lack of FDA-approved treatments for children.
Julie Khlevner, MD, Director of the Pediatric Gastroenterology Motility Center at NewYork-Presbyterian Morgan Stanley Children’s Hospital, presented a poster at DDW examining real-world prescribing patterns for pediatric patients with FC and IBS with constipation (IBS-C). The retrospective, observational study evaluated prescription patterns for both conditions across the U.S. using data de-identified from medical and pharmacy closed claims between January 2018 and June 2023. During that timeframe, approximately one-third of pediatric patients received prescription medication for constipation; polyethylene glycol 3350 (PEG) was the most frequently prescribed, followed by lactulose. Neither medication is currently FDA-approved for use in pediatric FC and IBS-C.
Dr. Khlevner noted that shortly after the study period, linaclotide, an intestinal secretagogue commonly used in adults with chronic idiopathic constipation and IBS-C, became the first FDA-approved treatment for pediatric FC in children six to 17 years of age. Dr. Khlevner suggests that future reevaluation of prescribing patterns in pediatric FC after this approval may provide additional real-world insights into treatment patterns.
Controversies in GERD Diagnosis and Management
Philip Katz, MD, a gastroenterologist at NewYork-Presbyterian and Weill Cornell Medicine and a leading expert on esophageal disease, presented during a session on multiple controversies in the management of gastroesophageal reflux disorder (GERD). He specifically discussed the role and need for pharmacologic therapy and why doctors must understand the contributing factors to GERD, including lower esophageal sphincter dysfunction, hiatal hernia, esophageal hypersensitivity, impaired esophageal clearance and delayed gastric emptying, among others.
Regarding treatment, Dr. Katz stressed that a personalized approach is ideal to improve quality of life, reduce and/or eliminate recurrence, and prevent complications. A discussion on the limitations of proton pump inhibitors (PPIs) served as a segue to a discussion of a new class of acid-reducing agents, potassium competitive acid blockers (PCABs). Dr. Katz highlighted the differences between PCABs and PPIs and the potential advantages of PCABs especially in the setting of erosive esophagitis, which have a different mechanism of action, a more potent and more rapid onset of acid control, are meal independent, and independent of genetic polymorphism.
Weight Loss Therapies for MASLD
Although metabolic dysfunction-associated steatotic liver disease (MASLD) affects up to 25% of people worldwide, there are few treatment options. Sonal Kumar, MD, MPH, Director of the Innovative Center for Health and Nutrition in Gastroenterology (ICHANGE) at NewYork-Presbyterian and Weill Cornell Medicine, shared her expertise in a session on weight-loss therapies for MASLD, specifically on weight-loss medications. She highlighted that MASLD is not just a disease of the liver but a metabolic process that is closely linked to other diseases such as obesity, diabetes, and cardiovascular disease.
For patients with MASLD, Dr. Kumar discussed the importance of lifestyle modifications, including diet and exercise, as fundamental to the management of the disease, even though achieving and sustaining significant weight loss can be challenging for some people. In patients with evidence of fibrosis, who subsequently have a higher risk of liver-related complications, Dr. Kumar asserted that anti-obesity medications can be a useful tool, with the strongest histologic data supporting the use of GLP-1s in patients with MASLD.
Endoscopic Evaluation of the Post-Surgical Bowel
Approximately 70% to 80% of patients with Crohn’s disease and 10% to 15% of patients with ulcerative colitis require surgical therapy despite advances in medical treatment over the past two decades. These resective or reconstructive surgical procedures result in significant changes in the bowel anatomy. During a session on endoscopic challenges in IBD, Bo Shen, MD, Director of the IBD Center and Co-director of the Global Center for Integrated Colorectal Surgery and IBD Interventional Endoscopy at NewYork-Presbyterian and Columbia, acknowledged the role that endoscopy plays in the monitoring of disease recurrence and treatment of post-operative complications — however, post-surgical diagnostic and therapeutic endoscopy can be challenging because of the anatomical changes. In his presentation, he highlighted the typical postoperative anatomy and common locations of recurrent disease and guidance for proper management of surgery-associated complications.
Identifying Microbiologic Mechanisms in Iron Deficiency in Quiescent Pediatric Crohn’s Disease
Elliott Gordon, MD, MSc, FAAP, a pediatric gastroenterologist at NewYork-Presbyterian and Weill Cornell Medicine, presented a poster looking at the microbiologic mechanisms at play in quiescent pediatric Crohn’s disease with iron deficiency.
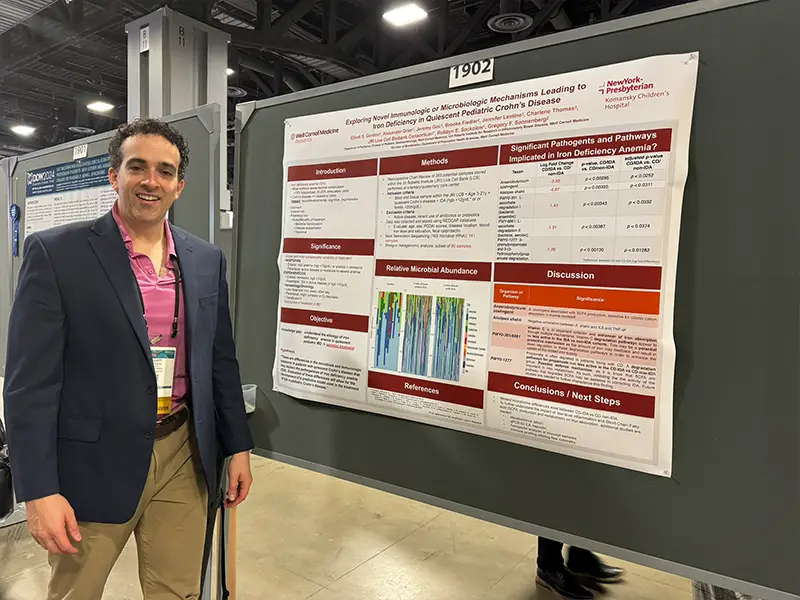
Dr. Gordon’s research focused on the microbiologic mechanisms that may play a role in iron deficiency in quiescent pediatric Crohn’s disease.
On microbiome analysis, Dr. Gordon found lower abundance of two bacteria implicated in short-chain fatty acid (SCFA) metabolism, while three pathways involved in SCFA or vitamin C metabolism and less active in this population. This suggests that there is something inherently different in the microbiome of those with iron deficiency versus those without. Additionally, Dr. Gordon explained that the microbiome may hold some, but not all, of the answers regarding the underlying etiology of iron deficiency anemia in quiescent pediatric Crohn’s disease; future research may focus on immune-profiling patients to further understand this phenomena.
Key Takeaways
Drs. Khlevner, Katz, Shen, Kumar, and Gordon share some of their personal takeaways and highlights from this year’s DDW:
Dr. Khlevner: The top three things I took away from the presentations at DDW were about the progressive role of artificial intelligence in clinical care; the latest information about emerging dietary therapies for disorders of the gut-brain interaction (DGBI); and that restrictive eating is associated with worse nausea and other clinical outcomes in adolescents with DGBI.
DDW was also a perfect milieu for making important connections within the global GI community for future collaboration to advance discovery, promote innovation, and improve patient care and outcomes.
Dr. Katz: There were multiple updates this year in the diagnosis and treatment of GERD, achalasia, and Barrett’s esophagus. I also had the opportunity to evaluate emerging therapies and medical technology across my specialty.
Dr. Kumar: I was particularly excited to hear the results of three key studies in liver disease:
- In patients with MASLD and diabetes mellitus, one study showed that use of GLP-1s were associated with a reduction in risk of hepatocellular carcinoma or progression cirrhosis.
- Another study looked at long-term effects of stopping nucleoside analogue treatment in patients with hepatitis B without cirrhosis. Relapse rates were as high as 83% at 144 weeks, suggesting that most patients will not be able to stay off medications long-term.
- Interim results from the ASSURE study, an open label, phase 3 study of patients with primary biliary cholangitis (PBC), showed that seladelpar improved alkaline phosphatase, normalized alkaline phosphatase, and had an excellent safety profile. The anticipated approval of this new therapy is a great advancement in the field of PBC.
Dr. Shen: Learning, teaching, and exchanging ideas during DDW has tremendously advanced digestive disease science and patient care. Three things that I was particularly excited about this year included new medical therapies; new techniques, including AI and endoscopy; and new theories in the etiology and pathogenesis of digestive diseases.
Dr. Gordon: The opportunity that DDW offers trainees like me to partake in discussions, network, and learn from individuals at the top of their field is second to none. The biggest takeaways for me were that collaboration is critical to move the needle in GI research; AI-powered tools for both research and clinical decision-marking are an area to watch over the next one-to-five years; and precision-based medicine is the new frontier and not far from our reach.






