As a medical student in 1996, neurosurgeon Raymond F. Sekula, Jr., MD, recalls the moment he first became aware of trigeminal neuralgia. “An elderly African American man with chronic high blood pressure who had been cared for by his internist for years presented with a new complaint,” says Dr. Sekula. “The patient reported that for several weeks he felt like fire was shooting through his face when he ate or spoke. Benign triggers included cool wind, brushing his teeth, and shaving. Looking at me he said, ‘The pain can bring me to my knees, son. It’s so bad, it makes me cry.’ On that day, he presented with half of his face unshaven. His gifted and kind internist diagnosed him with trigeminal neuralgia and prescribed a course of carbamazepine. I still remember the first follow-up appointment when the patient, with a neatly shaven face, reported to the internist, “It’s gone, doc...it’s a miracle.”
Dr. Raymond Sekula
That early introduction to trigeminal neuralgia set Dr. Sekula on a course that would define his neurosurgical career. In February 2022, Dr. Sekula joined the Department of Neurological Surgery at NewYork-Presbyterian/
One of the world’s foremost leaders in minimally invasive brain surgery and cranial nerve disorders, including trigeminal neuralgia (TN), hemifacial spasm, and glossopharyngeal neuralgia, Dr. Sekula has performed more than 5,000 neurosurgical operations in his career, including more than 2,000 microvascular decompression surgeries with patients seeking out his expertise from throughout the country and around the world.
“While that first patient I witnessed was likely suffering with classical trigeminal neuralgia, many patients experience TN in various forms that we do not understand as well as we would like,” says Dr. Sekula. “Unfortunately, for many patients, the story is more complex, more nuanced. And, unfortunately even for many patients with classical TN, medications often lose their effectiveness with time.”
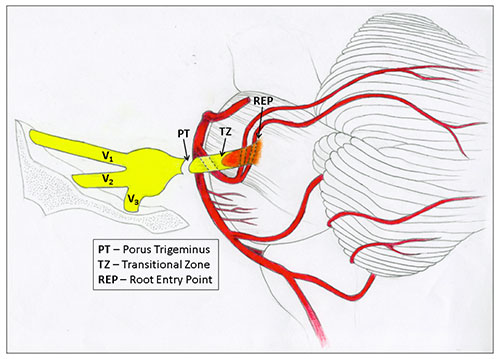
TN is a form of neuropathic pain of the trigeminal or 5th cranial nerve, starting near the top of the ear and splitting toward the eye, cheek, and jaw. The pain is often described as stabbing, lancinating, or electrical in sensation and so severe that the person cannot eat or drink. The pain travels through the face in a matter of seconds or as long as two minutes and may occur numerous times each day with periods of days to months of remission. The pain can be physically and mentally debilitating. Triggers include innocuous stimuli such as a light touch, wind, or chewing.
“All patients with classical trigeminal neuralgia will benefit from a neurosurgical consultation,” says Dr. Sekula. “Approximately 85 percent of patients with this disorder will have evidence of some degree of vascular compression of the trigeminal nerve via MRI imaging. And that degree is important in making the best recommendation and can only be determined with a high-resolution 3-Tesla MRI. Here at Columbia, we have seven 3-Tesla MRI machines with the highest-quality resolution to detect and assess the features of neurovascular compression.”
In the depiction below of the trigeminal nerve and brainstem, the artery (red structure) is compressing the trigeminal nerve (yellow structure).
According to Dr. Sekula, a patient’s response to the anticonvulsant medications carbamazepine or oxcarbazepine also provides helpful information for the clinician. “Many patients report rapid relief of facial pain within just minutes of the first tablet or two of these drugs,” he says. “While we do not fully understand why response to the drugs is an important predictor of response to neurosurgical intervention, we do know that it is important.”
Role of Microvascular Decompression
Dr. Sekula and his colleagues developed the following quantitative grading system to aid patients and referring clinicians in understanding if MVD is the optimal choice.
| TN Grading System Score* | Estimated Probability of Long-Term Pain-Free Status (95% CI) |
|---|---|
5 | 93% (0.92 - 0.93) |
4 | 76% (0.74 - 0.78) |
3 | 44% (0.40 - 0.47) |
2 | 16% (0.12 - 0.21) |
1 | 4% (0.03 - 0.06) |
*Derived from adding points from 3 characteristic categories, points assigned as follows:
| TN Type | Response to Carbamazepine or Oxcarbazepine | Neurovascular Contact |
|---|---|---|
Classical | Yes | Arterial Deformation |
Non-Classical | No | Arterial Contact |
|
| Absent or Venous Contact |
In addition to TN, Dr. Sekula has developed minimally invasive surgical techniques for glossopharyngeal neuralgia, which is associated with repeated episodes of severe pain in the tongue, throat, ear, and tonsils, and hemifacial spasm, another rare and chronic condition that causes involuntary muscle twitches on one side of the face.
“Microvascular decompression works well for many, but not all, patients with classical trigeminal neuralgia,” says Dr. Sekula. “It does not work for TN secondary to multiple sclerosis or cluster headaches. For these patients, we have other techniques to help them. MVD works particularly well for glossopharyngeal neuralgia patients. Sometimes, MVD can be used in combination with patients who have tumors compressing their trigeminal nerve.”
Dr. Sekula has refined many of the surgical techniques of MVD, and the surgery is associated with minimal blood loss. “It’s a gentler surgery so that patients do not require an intensive care unit stay and are discharged from the hospital in a day or two, which formerly was unheard of,” he says. Because the incidence of TN increases with age, neurologists and neurosurgeons frequently encounter elderly patients with this disorder. Although MVD is the only etiological therapy for TN with the highest initial efficacy and durability of all treatments, it has nonetheless been associated with risks not seen with commonly performed ablative procedures. “Previously it had been thought you wouldn’t perform MVD in individuals over the age of 65 because it was too dangerous,” says Dr. Sekula. “I’ve worked very hard to make this a safer surgery so that if a patient is older and generally healthy, MVD is still the best procedure as it rids them of pain and it doesn’t cause other complications or deficits.”
Dr. Sekula’s clinical practice parallels a prolific academic career that includes authorship of over 100 scientific manuscripts, and as editor of the textbook, Microvascular Decompression Surgery. Currently, he and his scientific partner, Michael Gold, PhD, are collaborating on a five-year $3 million drug discovery grant from the NIH to investigate the fundamental mechanisms of trigeminal neuralgia. As a Principal Investigator, Dr. Sekula hopes, “that the results of this work will form the basis for viable medications to help those individuals who cannot be helped with available medications or surgery.”
Dr. Sekula co-founded the World Federation of Cranial Nerve Disorders in 2016, and he is a member of the Medical Advisory Board of the Facial Pain Association, an international association dedicated to helping patients with facial pain of all types.
“Over the years I’ve treated patients with all forms of trigeminal neuralgia. In particular, we are concentrating on patients with facial and throat pain who have not been helped in the past. Many have been on medications for years,” adds Dr. Sekula. “These patients could well benefit from a neurosurgical consult and MVD.”