According to Srikanth Reddy Boddu, MD, an interventional neuroradiologist at NewYork-Presbyterian and Weill Cornell Medicine and director of interventional neuroradiology at NewYork-Presbyterian Queens, the incidence of idiopathic intracranial hypertension (IIH) is likely underestimated in scientific literature. While it is estimated to be one to two per 100,000, Dr. Boddu sees 150 to 200 patients yearly and is one of only a few clinicians in the country who can treat the condition using minimally invasive techniques. Dr. Boddu shares more about his experience treating IIH and discusses his recent article published in World Neurosurgery about the benefits and challenges of using venous sinus stenting (VSS) for treatment of IIH and pulsatile tinnitus.
What Causes IIH?
This is a pathology more commonly seen in female patients with obesity that creates increased pressure inside the head. The cause of this condition was unknown for a long time, but we now know that 93% of these patients have venous sinus stenosis, a narrowing that prevents clearing of the cerebral venous blood out of the brain. Symptoms vary from pulsatile tinnitus, a whooshing or a pulsing noise in the ears, to headaches and a gradual decline in vision. In more advanced stages, the condition can impact deeper functions like cognition, memory, and balance.
Barriers to Care
A general lack of awareness of idiopathic intracranial hypertension leads to the condition being underdiagnosed. Beyond this, not every patient presents with symptoms matching the textbook definition, making it more challenging for physicians to recognize IIH. Patients often see several doctors who attempt to treat their symptoms but don’t address the underlying problem causing them. Further, 90% of practicing physicians are trained in arterial versus venous treatments. Therefore, even if patients do get treatment for IIH, most physicians opt for ventriculoperitoneal (VP) shunts, which are associated with poor outcomes.
Challenges With the Standard of Care
Pharmacologic treatment of IIH is associated with side effects, including “pins and needles” in the arms, exhaustion, dehydration, stomach cramps, and increased urgency to use the bathroom. The other treatment option is a VP shunt, which is an open surgical approach where a plastic tube drains fluid from the brain to the patient’s stomach. The challenge with this procedure is that nearly half of the shunts placed will fail after two years, requiring patients to undergo additional procedures. Additionally, this tube connects the most sterile part of our body, the brain, with the most unsterile, the abdomen, putting patients at risk of meningitis.
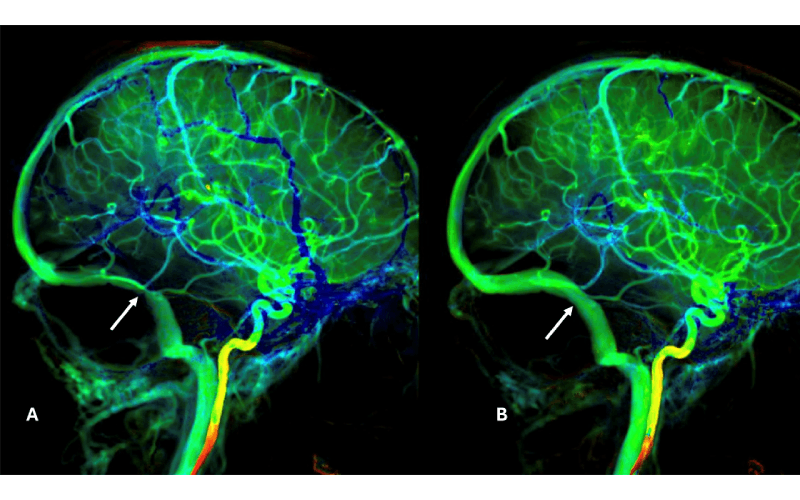
A: Lateral view of the brain angiogram showing the site of severe venous sinus stenosis (white arrow) before [A] and after [B] stenting. Notice a short segment of severe narrowing of the vein [A] before treatment and a wide-open vein with resolution of narrowing after treatment with a single stent [B]
Advancing Care With Venous Sinus Stenting
Venous sinus stenting is a minimally invasive technique that effectively treats IIH. To select the right patients for venous sinus stenting, preoperative evaluation is critical. Patients are evaluated during the clinical visit using magnetic resonance venography to visualize the stenosis; a venogram and manometry can also be used to measure the pressures and further determine candidacy. The procedure involves placing a stent by threading a catheter up into one of the narrowed veins in the brain; the catheter can be inserted through a standard IV line in the arm. The stent is delivered via the catheter and deployed at the narrow point in the vein. The widened vein allows excess cerebrospinal fluid to drain at a more normal rate, relieving the pressure. Given the minimally invasive nature of this procedure, patients can often go home the same day or the following morning.
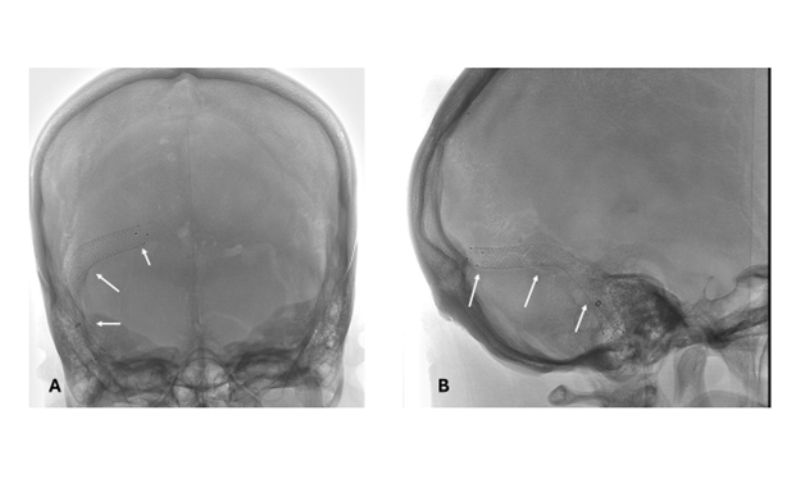
Visualization of the right sided venous sinus stent (white arrows) on frontal [A] and lateral [B] projections.
At NewYork-Presbyterian Queens, Dr. Boddu and his established team have done so many of these procedures that the entire process is streamlined, efficient, safe, and effective. It is associated with a less than 1% risk of complications, and meta-analyses suggest this technique is the most effective treatment option for IIH patients. Further, the procedure offers immediate relief for patients with pulsatile tinnitus and can resolve vision issues within three months.
The Challenges That Remain
There are still many challenges to the widespread use of VSS to treat idiopathic intracranial hypertension. First, there is no universal agreement on candidacy requirements. While most physicians agree that failed medical treatment and pressure gradients indicate candidacy, they disagree on whether medical refractoriness is required. Further, clinicians disagree on what tool is the best for diagnostic imaging. There are also challenges with the VSS technique, including a steep learning curve, stent choice, and deployment. Finally, there is insufficient evidence surrounding postoperative decision-making regarding postprocedural balloon angioplasty and pharmacologic therapy. Despite these challenges, evidence suggests that VSS is still the best treatment option for IIH patients.




