Tumor-associated seizures (TAS) often do not respond to antiseizure medications and can be highly debilitating. Moreover, in the case of gliomas, evidence suggests that seizure-induced neuronal hyperactivity can promote tumor progression. Neurosurgeons at NewYork-Presbyterian/

Brian Gill, MD
"Seizures in people with glioma are potential drivers of tumor progression and recurrence. They are undertreated and may play a role in a patient's disease beyond clinical symptoms," explains Brian J.A. Gill, MD, a neurosurgeon at NewYork-Presbyterian/
While the mass of a tumor can contribute to seizures, there are signaling changes at the molecular level that occur due to the presence of the tumor and how it communicates with healthy neurons. "Those conversations drive seizures. They alter normal neuronal function as well as patient function, leading to adverse effects on speech, cognition, and motor function," Dr. Gill notes. "But then these conversations are highjacked to drive tumor growth, so understanding them is vitally important. How does this crosstalk drive tumor progression and recurrence, and what can we learn from these interactions to treat brain tumors?"
By treating seizures in someone with glioma, there could be an opportunity to improve quality of life while also contributing to oncologic care.
— Dr. Brian Gill
Dr. Gill has been studying brain tumor biology since he was a medical student at Columbia University Vagelos College of Physicians and Surgeons. He became especially interested in the brain tumor cells that are left behind when a tumor mass is resected, cells that remain distributed throughout the brain but cannot be removed. While attending a conference with co-investigator Peter Canoll, MD, PhD, a NewYork-Presbyterian/
Using techniques called single unit analysis and wide-field imaging, Drs. Gill and Canoll and their NewYork-Presbyterian/
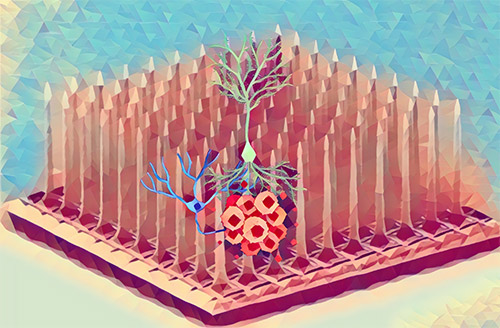
A graphic rendering featuring tumor cells (red) and neurons (blue and green), undergoing electrophysiologic recording on a microelectrode array.
They found that in the presence of tumor cells, inhibitory neurons fire much less frequently and tend to fire in concert with excitatory neurons, contributing to seizure-like events. They also observed that excitatory neurons were activated by inhibitory firing. Dr. Gill and his team then applied AZD8055, a dual-acting mTOR inhibitor that can cross the blood-brain barrier, and discovered that the use of this medication could reverse this process. AZD8055 restored the firing of inhibitory neurons and dialed back the activity of excitatory neurons, corresponding to a reduction in seizure activity.
"We know that mTOR inhibitors are useful for treating seizures in people with tuberous sclerosis complex but not for treating glioma. But no one has ever shown that inhibitory neuronal dysfunction in people with brain tumors can be reversed in the presence of an mTOR inhibitor," said Dr. Gill. "While this is not a cure, it could potentially reduce seizure activity in people with glioma and, by extension, slow tumor progression."
Understanding the conversations that brain tumor cells have with their microenvironment and how we can leverage those interactions to improve care is the next frontier.
— Dr. Brian Gill
Next steps: to evaluate the use of AZD8055 in vivo in mice with brain tumors to assess its effects on seizure frequency and tumor progression. The investigators also want to explore interictal discharges—abnormal neuronal activity that may frequently occur in the region of a tumor—to see how they influence tumor progression. Some of the same molecular changes that lead to seizures may be occurring during those interictal discharges, so stopping them has the potential to inhibit tumor growth.
"We've done a great job learning more about brain tumor biology," Dr. Gill concluded. "Now we want to better understand the conversations that residual tumor cells are having with their surrounding microenvironment and how we can leverage those interactions to improve brain tumor care. That's the next frontier."




