Small for gestational age (SGA) newborns weigh less than the tenth percentile for their gestational age and sex. Preterm SGA babies in neonatal intensive care units (NICUs) are the infants who most often experience critical illness and die, but the mechanisms underlying these outcomes are poorly understood. A new study looking at the outcomes of more than 200,000 early preterm infants has demonstrated a link between genetic disorders and morbidity and mortality in early preterm SGA infants.
Conducted by Thomas Hays, MD, PhD, a neonatologist at NewYork-Presbyterian and Columbia, Columbia medical student Miles Bomback, MPH, and their colleagues, the study retrospectively analyzed national NICU data to show how genetic disorders boosted the risk of SGA in preterm newborns, especially in babies with congenital anomalies. Below, Dr. Hays elaborates on the study findings and the potential role genetic testing could play in the care for SGA preterm infants.
Research Background
Low birthweight early preterm infants may have a lower metabolic reserve or other factors that explain much of their illness, but it doesn't explain all of it. We also don't know why these babies are born with low birth weights. We can find some causes related to maternal comorbidities, such as high blood pressure or diabetes, but again, this explains only a fraction of the overall incidence of SGA.
Studies of babies who become ill or die in the NICU have found very high rates of Mendelian genetic disorders — those that are either inherited or occur as a new mutation. However, current guidelines are a little vague about when we should be doing genetic testing in NICU infants. We hypothesized that genetic disorders are likely contributing to low birth weight in preterm infants and may explain why they become critically ill and die in the NICU.
Research Methods
We conducted a retrospective cohort study of infants delivered from 23 to 33 weeks gestation between 2000 and 2020. Using the Pediatrix Clinical Data Warehouse, we made a dataset of more than 400,000 early preterm infants from across the United States, which represented approximately 20% of all early preterm infants born in the United States during that period. After exclusions, we analyzed data on genetic disorders, congenital anomalies, baseline characteristics, and morbidity and mortality in the NICU for 223,431 infants— 21,180 of whom were SGA. Congenital anomalies included major birth defects such as congenital heart disease, structural anomalies of the kidneys, and rare disorders such as gastroschisis.
Infants diagnosed with genetic disorders were much more likely to be born SGA, and SGA infants with genetic diagnoses were much more likely to become critically ill.
— Dr. Thomas Hays
Key Findings
In a diverse, representative US cohort, genetic disorders were strongly associated with SGA birth. This was especially true for babies with congenital anomalies, morbidity or mortality. This association was driven largely by trisomies 13, 18, and 21, but other genetic disorders including many different pathogenic copy number variants and single gene disorders also contributed. Infants diagnosed with genetic disorders were much more likely to be born SGA, and SGA infants with genetic diagnoses were much more likely to become critically ill.
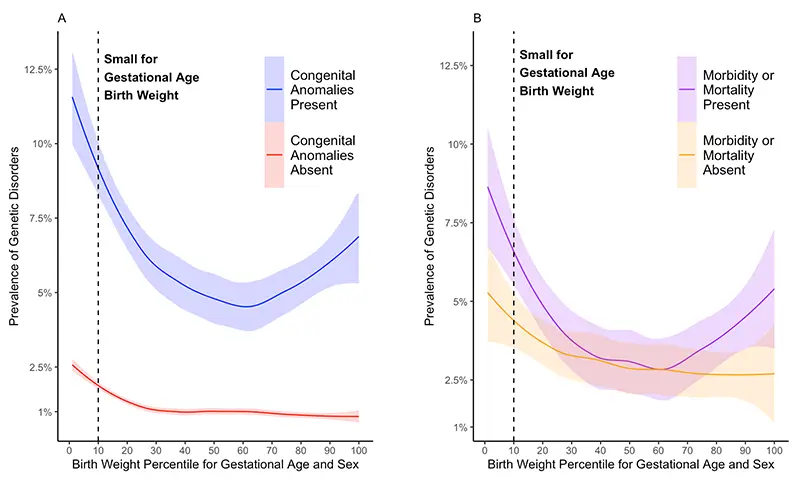
Proportion early preterm infants with genetic disorders versus birth weight
Overall, genetic disorders were present in:
- 2.3% of early preterm SGA infants without congenital anomalies versus 1.0% of appropriate for gestational age infants without congenital anomalies
- 10.8% of early preterm SGA babies with congenital anomalies versus 5.8% of appropriate for gestational age infants with congenital anomalies
- 4.5% of early preterm SGA infants who became sick or died in the NICU versus 2.0% of appropriate for gestational age infants who became sick or died
Future Implications
At NewYork-Presbyterian, there is incredible strength in neonatal care and research. We have a great history of improving neonatal management and a group that's dedicated to innovating and improving newborn care. As a regional referral center for a large area with extraordinary leadership in neonatology, maternal-fetal medicine, and genomics, we attract many cases, enabling us to do the type of prospective genomic research needed to further explore these findings.
Our findings demonstrate that genetic disorders are more prevalent in early preterm SGA infants, especially those with congenital anomalies or critical illness. Our data support the consideration of genetic testing and consultation with colleagues in clinical genetics for early preterm SGA infants. They also suggest that we need prospective genomic research to define the true prevalence of genetic disorders in this population.




