Women with type 2 diabetes are at increased risk for fracture; however, the mechanism behind these fractures is unclear and very few population-based studies address this issue. To better understand this occurrence, Marcella Walker, MD, an endocrinologist at NewYork-Presbyterian and Columbia, worked with Edward Guo, PhD, director of Columbia’s Bone Bioengineering Laboratory, Sanchita Agarwal, MS, a biomedical engineer and clinical research data analyst, and additional Columbia colleagues to conduct a multi-ethnic, population-based study to investigate bone microstructure, trabecular plate/rod morphology, and mineralization in elderly women with type 2 diabetes with and without fracture.
A Confounding Clinical Scenario
Why do individuals with type 2 diabetes (T2DM) have a higher risk of fracture even when their bone density, as measured by DXA, is higher on average than people who do not have diabetes? To answer this question, Dr. Walker and the research team decided to move beyond bone density measurements to investigate the microstructure of bone. To accomplish this, they employed second-generation high-resolution peripheral quantitative computed tomography (HR-pQCT) and other state-of-the-art methodologies that would enable them to identify deficits in cortical parameters and trabecular plates. “Our goal was to assess bone strength and the differences in microstructure that might explain increased risk of fracture in people with T2DM,” says Dr. Walker. “While HR-pQCT is frequently used in musculoskeletal research, it had not been applied extensively for understanding fractures related to type 2 diabetes.”
Understanding how these processes are regulated in human beta cells is an important ground floor for all kinds of exciting potential features.
— Dr. Laura Alonso
The research team also utilized individual trabecula segmentation and mineralization analysis to complete skeletal characterization. These novel analysis methods, developed by Dr. Guo, quantify microstructural morphology and the tissue mineral density of each trabecula to detect changes in tissue material properties among other properties, potentially implicated in the pathogenesis of skeletal fragility in T2DM.
The study utilized participants from the Washington Heights Hamilton Heights Inwood Community Aging Project, a longitudinal study of aging among elderly urban-dwelling residents in the racially and ethnically diverse Northern Manhattan communities served by NewYork-Presbyterian and Columbia. The cohort population included in this analysis was 31% Black, 26% White, 42% mixed race, and 55% Hispanic.
Key Findings
The study cohort included 565 women with a mean age of 76.8. Of these, 175 women had type 2 diabetes and 59 participants had a history of adult fragility fracture. In comparing skeletal health data, the researchers findings demonstrated:
- Participants with T2DM tended to have higher bone density and better bone structure measured by DXA and HR-pQCT, respectively, at the radius and tibia, except for cortical porosity
- Cortical porosity was increased (worse) in those with T2DM, but there was no difference in bone strength between the two groups
- Women with T2DM who have had a fracture had marked cortical deficits, lower plate volume, and lower failure load or bone strength
Enhancing the Knowledge Base
An interesting aspect of this study involved assessing bone health in those using sodium-glucose cotransporter 2 inhibitors (SGLT2i), a newer class of drugs now being used for diabetes. “In some studies, but not others, these drugs have been associated with an increased risk of fracture; however, information is lacking on how they might affect the microstructure or material properties of bone,” says Dr. Walker. “Therefore, we also looked at a subset of people on these medicines to see whether they had additional skeletal insults. The results suggest some differences in bone material, and we were the first to describe that finding.”
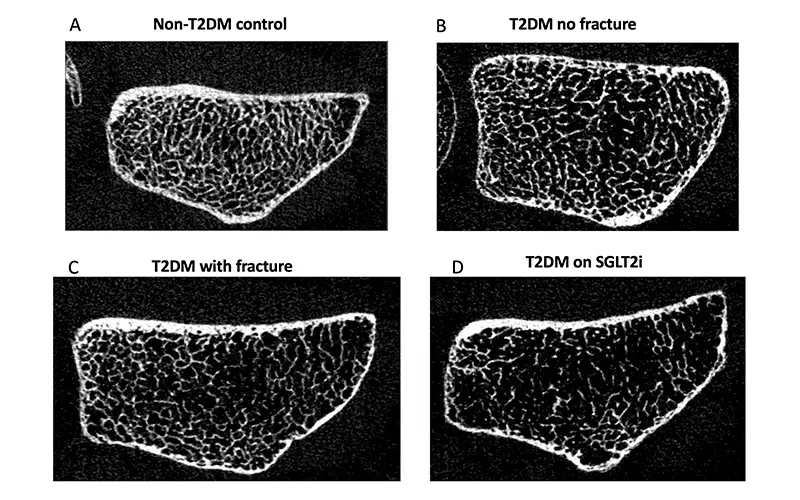
Representative HRpQCT images in (A) control with no diabetes, (B) woman with diabetes without fracture, (C) woman with diabetes with fracture, (D) SGLT2-inhibitor user.
The study also evaluated 19 people taking GLP-1 receptor agonists (GLP1-RA). The researchers found some deterioration of bone microstructure associated with the use of this medicine as well. “Weight loss in general will cause bone loss,” says Dr. Walker. “On top of that, is there an independent effect of the drug on bone? That is important to tease out.”
Study participants on SGLT2i tended to have lower radial rod tissue mineral density. Those taking the GLP1-RA had trabecular deficits at both sites and higher cortical porosity and larger pores at the distal tibia. Further research is needed to understand the pathophysiology by which SGLT2iand GLP1-RA may affect bone metabolism.
Future Implications
“To our knowledge, our study cohort represents the largest group of patients with T2DM assessed with HR-pQCT and the only study to examine effects of SGLT2i and GLP-1 RA use on bone health using this technology,” says Dr. Walker. “Going forward, a prospective study showing that the bone microstructural deficits that we identified predict future fracture would be helpful.”
The researchers are currently collecting prospective data on participants from the current study on whether or not they fractured during the follow-up period. That data will be used to determine whether the bone microstructure has the potential to be predictive of incident fractures. “With the evidence that people with type two diabetes are at increased risk of fracture, we want to reinforce the importance of screening,” says Dr. Walker.
Ms. Agarwal adds “DXA does not always tell the complete story of bone structure. Evaluating these patients more diligently provides us with the potential to prevent fractures.”




