
Dr. Alessio Pigazzi
NewYork-Presbyterian/
“The treatment has been utilized for over 20 years and is becoming increasingly more accepted,” says Dr. Pigazzi, who specializes in complex surgeries involving the colon, rectum, and anus. “Only a handful of cases were done at Weill Cornell over the last several years, but our case numbers are growing quite rapidly.”
How the Procedure Works
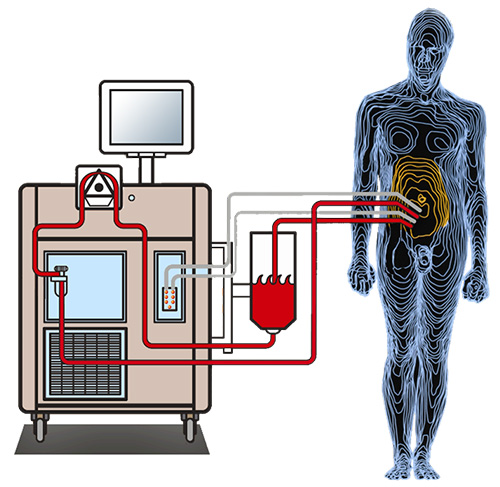
During the complex surgery, all visible evidence of disease is removed, known as cytoreduction. Then cannulas are inserted through the same incisions to instill chemotherapy heated to the temperature of bath water into the abdomen.
“A machine circulates the chemo in and out,” says Dr. Pigazzi. “It’s similar to a heart lung machine but with just a simple pump and a heating component.”
Cytoreductive surgery followed by HIPEC is a comprehensive surgical treatment for certain patients with malignancies arising from or confined to the peritoneal cavity.
The patient’s belly is gently rocked and massaged to allow the chemotherapy to coat the peritoneal surface and kill any microscopic cancer cells. After about an hour and a half, depending on the type of agent used, the solution is drained from the abdomen and the procedure is completed.
We maximize the potential therapeutic effects of both chemo and surgery by administering them at the same time.
— Dr. Alessio Pigazzi
Numerous benefits are associated with HIPEC. Heating the chemotherapy enhances its ability to penetrate cancer cells left after surgery. Because the chemotherapy is delivered directly to the abdomen, patients experience fewer side effects than systemic chemotherapy. At the same time, HIPEC allows a higher dose of chemotherapy to be used than through intravenous chemotherapy because the body absorbs it differently through the peritoneal walls.
“The goal is to really get everything out. If you do the surgery and leave disease behind, it's not going to be helpful,” says Dr. Pigazzi. “We maximize the potential therapeutic effects of both chemo and surgery by administering them at the same time.”
Recovery can be challenging, Dr. Pigazzi cautions. “It’s something we don’t take lightly,” he says. “So, we try to be extremely selective in who gets this procedure.”
Careful Patient Selection
Cytoreductive surgery and HIPEC is currently an option for primarily colorectal cancer, appendiceal cancer, peritoneal mesothelioma, pseudomyxoma peritonei, and other rare cancers invading the abdominal cavity. Not every patient with such cancers is a candidate for the treatment, however, Dr. Pigazzi says.
[The treatment is] best for patients who do not have a heavy burden of the disease and have low-grade tumors.
— Dr. Alessio Pigazzi
The ideal patient has tumor that has spread only to the peritoneal cavity and not to other organs, such as the liver or lungs. Dr. Pigazzi’s team looks for certain tumor characteristics that predict that the treatment could be beneficial. Colorectal cancer patients chosen for the surgery typically have been on systemic chemotherapy previously and responded well to it.
“It's best for patients who do not have a heavy burden of the disease and have low-grade tumors,” Dr. Pigazzi says. “And obviously they need to be fit to undergo the procedure. Only a small percentage of patients qualify.”
Before patients are committed to the surgery, potential candidates undergo a diagnostic laparoscopy. Doctors insert a tiny camera into the belly to examine the peritoneal cavity and evaluate the extent of disease. Each case is overseen by a multidisciplinary team, including surgeons, oncologists, pathologists, and radiologists, who discuss it at a tumor board where they develop a personalized treatment plan.
Safety and Efficacy
Complications from the surgery, such as infection, bleeding, or blood clots, occur in 20 to 30 percent of patients, Dr. Pigazzi says. Side effects from the chemotherapy are minor when administered directly to the abdomen.
“Overall, the treatment is very safe,” says Dr. Pigazzi. “It can be done with very acceptable morbidity to the patient population undergoing these procedures.”
Data on the technique is limited but growing. “It’s difficult to do large studies because it very hard to find a big cohort of patients that you can randomize to this type of treatment or conventional therapy,” says Dr. Pigazzi. “It looks like there is a benefit, but it's probably only in a subgroup of patients.” In the future, Dr. Pigazzi hopes to conduct additional research, including clinical trials for patients with peritoneal surface tumors.




