
Julie Khlevner, MD
Pediatric neurogastroenterology and motility (PNGM) conditions are highly prevalent and often debilitating. Accounting for approximately 30-40% of outpatient pediatric gastroenterology visits, PNGM disorders affect the enteric nervous system, which controls how the gastrointestinal (GI) tract functions. NewYork-Presbyterian/
NewYork-Presbyterian takes a multidisciplinary, comprehensive approach to treating PNGM and brings together a multidisciplinary team to care for each patient, both at Columbia and at NewYork-Presbyterian/
Under the PNGM umbrella (including disorders of the gut brain interaction) falls conditions such as esophageal motility disorders (i.e. achalasia), functional dyspepsia, oropharyngeal dysphagia, gastroparesis, gastroesophageal reflux disease (GERD), irritable bowel syndrome (IBS), fecal incontinence, functional constipation, functional diarrhea, functional nausea and vomiting, and pediatric intestinal pseudo-obstruction (PIPO), among others. Dr. Khlevner reports that, in her clinic, a few of the conditions appear more commonly. “The most common and the most prevalent ones [we see] are GERD, irritable bowel syndrome, functional constipation, functional dyspepsia, gastroparesis and functional nausea,” she says. “We do see cyclic vomiting syndrome, abdominal migraine, infant dyskinesia, and other infant functional GI disorders as well.”
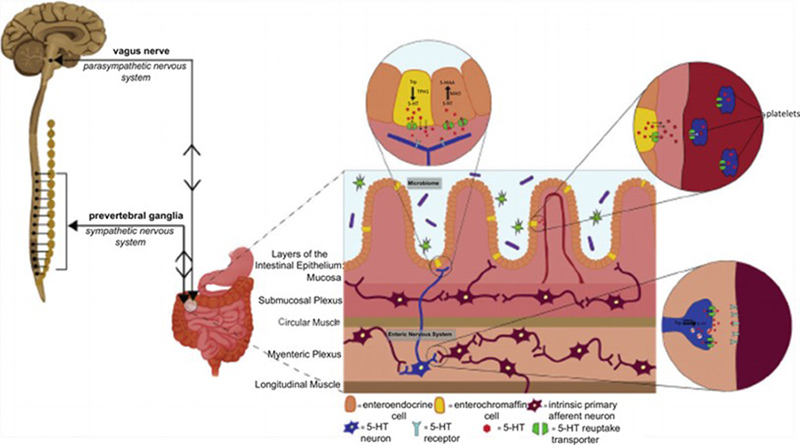
Complex bidirectional communication between the enteric nervous system and central nervous system (also known as the brain-gut axis) including the interplay with enteric microbiota and serotonin (5-HT). Image courtesy of Gastroenterology Clinics of North America.
Patients who come to NewYork-Presbyterian/
Depending on the diagnosis she’s treating, Dr. Khlevner may collaborate with speech language pathologists, pulmonologists, otolaryngologists, pediatric surgeons, psychiatrists, psychologists, dietitians, social workers, and others. “We involve every member of the team to really help patients get better,” she says.
Challenges of Diagnosing Neurogastroenterology and Motility Conditions
PNGM can be challenging to diagnose, given their development within a developing bowel and different pathophysiology than seen in adult patients, and require distinct diagnostic and management approaches that account for developmental age and the role of caregivers. “Patients with PNGM disorders are often misdiagnosed or undiagnosed because many pediatric gastroenterologists or advanced providers don’t necessarily get the training in these disorders,” Dr. Khlevner says. “There’s this perception by many that every organic disorder must be ruled out before a diagnosis of PNGM disorder is made. Those who are more familiar with PNGM are more comfortable diagnosing and embarking on treatment instead of just ordering more tests.”
Another key challenge to managing these conditions is understanding their overlap. “As our understanding of NGM disorders evolve, we are recognizing that some conditions have a significant overlap in pathophysiology, clinical presentation and treatment,” says Dr. Khlevner. “What we’re realizing [for example] is that functional dyspepsia may not be very different from gastroparesis. It’s likely a spectrum along the gastroduodenal neuromuscular disorders, and a patient may fall somewhere within the spectrum. A patient may be diagnosed with functional dyspepsia with delayed gastric emptying or gastroparesis with visceral hypersensitivity. There is definitely a case for considering these disorders as part of a spectrum where identification of both would most ideally position us toward providing the optimal clinical care.”
Despite the challenges of diagnosing these conditions, there have been advancements in the treatment of PNGM. “We are really expanding our knowledge about these disorders and looking into more innovative treatment options outside of just pharmacotherapy,” says Dr. Khlevner. “We’re more comfortable with nutraceuticals and other herbal supplements, percutaneous electrical nerve field stimulation, and other modalities that are outside of just medications prescribed by physicians.”
She adds that every diagnostic and therapeutic modality for PNGM is available to patients at NewYork-Presbyterian. “There is nothing that we don’t have,” she says. “We have the latest diagnostics and therapeutics including EndoFLIP (endoluminal functional lumen imaging probe), a complementary tool to high resolution manometry, which allows us to measure the distensibility and pressure of the esophagus and pylorus. We are using IB-Stim, a percutaneous electrical nerve filed stimulator, to help patients with IBS and functional nausea. These are some of the cutting-edge technologies that we have access to and the necessary expertise to offer to our patients. We are truly a one-stop shop and have enough expertise for these patients to not seek care anywhere else.”
“We are truly a one-stop shop and have enough expertise for these patients to not seek care anywhere else.” — Dr. Julie Khlevner
The Role of Diagnostic and Therapeutic Endoscopy in PNGM
One area of significant advancement over the past decade is in the use of diagnostic and therapeutic endoscopic modalities in PNGM. Editors at Gastrointestinal Endoscopy Clinics of North America approached Dr. Khlevner and two of her colleagues to author a paper providing an overview of the uses of endoscopy in the diagnosis and treatment of PNGM. “There is a lot of interest in terms of what we can offer for patients [with endoscopy],” says Dr. Khlevner. “This is an important paper that provides an overview of what’s available in pediatrics.”
The paper, published in March 2023, provides an overview of gastrointestinal endoscopic modalities and the emerging role of therapeutic and diagnostic endoscopy in the treatment of esophageal, gastric, small bowel, colonic, and anorectal disorders, and disorders of the gut brain axis interaction (DGBI).
In the paper, Dr. Khlevner and her co-authors outline different PNGM conditions and summarize the role of diagnostic and therapeutic endoscopy for each. Of note, the authors concluded that:
- Functional lumen imaging probe (FLIP) and EsoFLIP are important diagnostic and therapeutic tools for esophageal motor disorders.
- Intrasphincteric botulinum toxin injections may provide temporary symptom relief and/or help confirm certain esophageal and motility disorders, like cricopharyngeal dysfunction, achalasia, and gastroparesis.
- Intrapyloric botulinum toxin injections can be used in gastroparesis or in those with feeding difficulties who are failing medical therapy and not tolerating enteral feedings.
- Pneumatic dilation is therapeutically useful in upper GI disorders, such as peptic strictures, cricopharyngeal dysfunction, achalasia, and gastroparesis; however, there is a lack of consensus regarding duration and frequency of dilations or diameter that should be achieved in pediatric patients.
- There is a lack of evidence-based guidelines for the pediatric use of peroral endoscopic myotomy (POEM), gastric-POEM, transpyloric stenting, and electrocautery incisional therapy (EIT).
- Caution must be taken when using novel modalities, like FLIP, POEM, gastric-POEM, and EIT, due the need for an experienced endoscopist to perform the procedures and the paucity of available pediatric data.
- In achalasia, POEM is an effective alternative to pneumatic dilation and Heller’s myotomy; however, reflux remains a long-term concern and requires ongoing endoscopic surveillance for esophagitis.
- Endoscopic placement of manometric catheters can be advantageous as it minimizes the radiation dose and allows for simultaneous evaluation of mucosal disease and anatomical issues.
“Endoscopy has an emerging role in these disorders,” Dr. Khlevner says. “For example, Heller myotomy has been considered the definite surgical treatment for achalasia, a rare esophageal motor disorder due to aperistalsis and failure of lower esophageal sphincter relaxation with swallows. However, peroral endoscopic myotomy (POEM) is now an option for definitive treatment and saves the patient an invasive surgery.”
Finding an Expert in PNGM
Recognizing the need for more medical training in PNGM, Dr. Khlevner, who serves as the co-chair of Neurogastroenterology and Motility Committee of the North American Society of Pediatric Gastroenterology, Hepatology, and Nutrition (NASPGHAN), helped develop guidelines for PNGM training in North America.
Dr. Khlevner worked with other pediatric neurogastroenterologists, NASPHGHAN, and the American Neurogastroenterology and Motility Society (ANMS) to establish a task force to identify the entrustable professional activities (EPAs) a pediatric gastroenterologist, neurogastroenterologist, and/or motility expert should be capable of performing. The task force defined the core knowledge and skills necessary for each EPA as well as identified the diagnostic and therapeutic procedures clinicians should be able to perform and/or interpret associated with the EPAs. This new curriculum was published in the Journal of Pediatric Gastroenterology and Nutrition in January 2021.
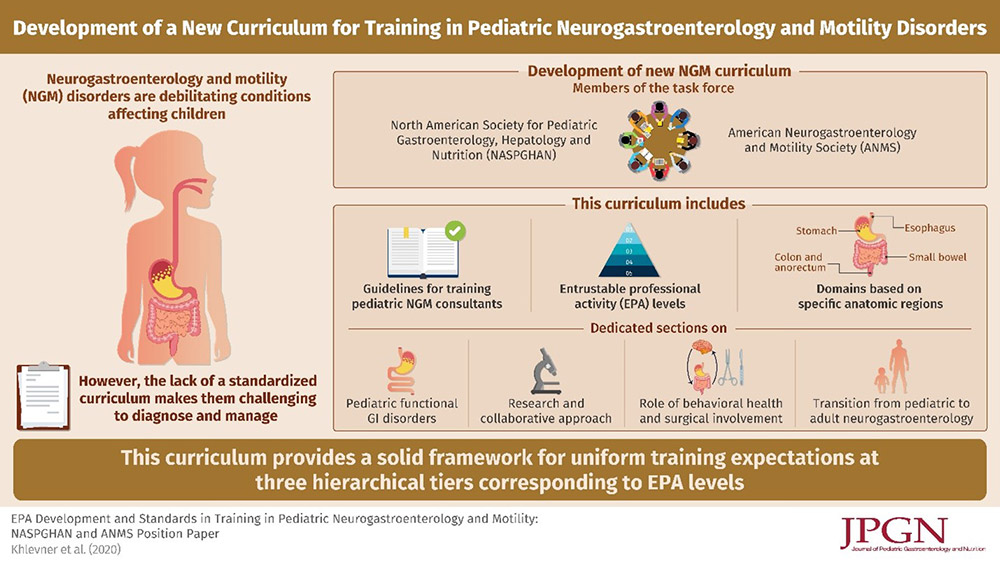
Summary of the rationale for developing a new PNGM curriculum and what it includes. Image courtesy of the Journal of Pediatric Gastroenterology and Nutrition.
In addition to establishing these guidelines, Dr. Khlevner worked with her colleagues to develop a database of centers offering pediatric neurogastroenterology and motility services in North America. A targeted survey was sent to NASPGHAN and pediatric gastroenterology listserv members. The results of the survey were published in the Journal of Pediatric Gastroenterology and Nutrition in May 2022 and found that:
- There are 54 unique PNGM centers in the United States, Canada, and Mexico
- 60% of states in the United States lack a PNGM center
- Almost all (94%) PNGM centers are based at academic/teaching institutions
- Five centers offer a 1-year advanced non-ACGME-accredited but Graduate Medical Education-approved PNGM fellowship
- 70% of the centers had more than 1 PNGM specialist; 30% had just 1
- 33% (19) of the centers reported conducting PNGM clinical research; of those 10 also perform translational research and 6 conduct basic science research as well
“This paper is a great resource for providers across North America. It is easy to navigate and get a sense of the PNGM landscape. Provider should not feel siloed in caring for children with PNGM. Even if there is no direct access to an PNGM expert in the immediate region, providers can locate the nearest PNGM center and ask for advice.” says Dr. Khlevner. “We’re always happy to review the case and give an idea of when it’s appropriate to refer to a neurogastroenterologist.”
Looking Toward the Future of PNGM Diagnosis and Treatment
Dr. Khlevner is hopeful for the future of PNGM diagnosis and treatment. “There’s going to be more drugs approved for our pediatric patients,” she says. “We are understanding more about the enteric microbiota and its role in PNGM and how to manipulate it in an evidence-based and sophisticated way. I think that this may be the wave of the future of how we take care of these patients.”
She also notes that there will be updates to the Rome criteria, an international effort to create diagnostic and treatment guidelines for neurogastroenterology and motility disorders. The most recent version, Rome IV, was published in 2016, and work is underway to publish a new update – Rome V – in 2026. “Rome V will provide a comprehensive understanding of what these disorders are, how to take care of them, and how to diagnose them,” Dr. Khlevner says. “It’s going to be a very informative update, which I think is going to change the landscape of how we treat and diagnose our patients with functional GI disorders or disorders of the brain-gut interaction.”
“I think validating the patient and their family is really important. Whether you feel that they are experiencing mild, moderate, or severe symptoms, you can’t minimize that for the patient who’s experiencing it.” — Dr. Julie Khlevner
While research is underway and new guidelines are being developed, Dr. Khlevner notes that those who are treating patients with PNGM should take their symptoms seriously. “I think validating the patient and their family is imperative,” she says. “Whether you feel that they are experiencing mild, moderate, or severe symptoms, you can’t minimize that for the patient who’s experiencing it. So validating it and understanding how that impacts their quality of life and providing an individualized and multidisciplinary approach is key for a successful outcome.”




