Eosinophilic esophagitis (EoE) is one of the most common allergic gastrointestinal conditions affecting children. It’s characterized by having an increased amount of eosinophils in the esophagus caused by an inflammatory response to specific foods and environmental allergens. Symptoms of EoE mimic those of other conditions – vomiting, failure to thrive, dysphagia, esophageal stricture, and others – so obtaining an accurate diagnosis and monitoring treatment is essential.
For children with EoE, undergoing esophagoscopy is a regular part of their routine. “Frequent esophagoscopies are required to monitor response to therapy,” says Ali Mencin, MD, Chief of the Division of Pediatric Gastroenterology, Hepatology and Nutrition at NewYork-Presbyterian/Columbia. “This could mean up to five or six esophagoscopies in a year, and all of them require anesthesia.”
Exposure to anesthesia comes with some risks, and the idea of exposing children to risks multiple times a year can be daunting for parents. “There are two risks to anesthesia. One is the concern of cumulative exposure to anesthesia from frequent procedures. But there is also a small risk whenever someone is sedated” says Dr. Mencin, who is also the Director of Pediatric Endoscopy at NewYork-Presbyterian/Columbia. “We know that when we put somebody to sleep there can be anesthesia related complications. These are very rare but a concern.”
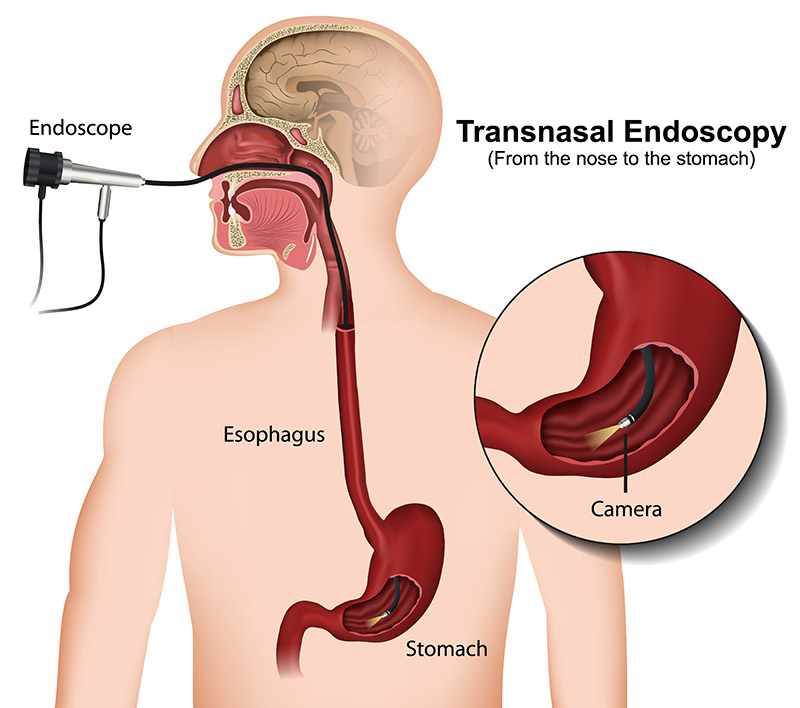
Dr. Mencin recognized these concerns and sought alternative options for monitoring of EoE without the frequent exposure to anesthesia. That led him to pursue the adoption of a new technique for pediatric patients – unsedated transnasal endoscopy (TNE). Under his leadership, NewYork-Presbyterian/Columbia is the first location in New York to offer this procedure to patients.
The adoption of unsedated TNE is just one of the many ways that NewYork-Presbyterian is committed to providing the best possible care to patients. “We want to make sure that the gastrointestinal care provided to children in New York City is at the highest level, and that involves utilizing innovations like transnasal endoscopy.”
We want to make sure that the gastrointestinal care provided to children in New York City is at the highest level, and that involves utilizing innovations like transnasal endoscopy.
— Dr. Ali Mencin
The Difference Between Unsedated Transnasal Endoscopy and Traditional Esophagoscopy
A traditional esophagoscopy takes about 30 minutes during which the physician inserts a mouthguard to protect the patient’s teeth and then guides the endoscope through the mouth and down into the esophagus. Preparation for an esophagoscopy involves having nothing to eat eight hours before the procedure due to the use of anesthesia. Additionally, patients are limited in what they can and cannot do the rest of the day after the procedure due to the use of sedation.
Both standard esophagoscopy and TNE allow physicians to view the lining of the esophagus, take distal and proximal esophageal biopsies. However, an unsedated TNE differs from an esophagoscopy in several important ways.
The first difference is the size of the endoscope used – while a standard pediatric endoscope has a 9.5 mm outer diameter, the TNE is 3.5 mm. The significantly narrower diameter allows the TNE scope to pass through the small nasal canal of children.
Preparation for TNE differs greatly as well. For an unsedated TNE, patients refrain from solid food for only four hours before the procedure and clear liquids for two hours. “The amount of time that’s required to prepare for the procedure is much less because you don’t have to be fasted overnight,” says Dr. Mencin.
Patients arrive at the endoscopy suite and have their vitals and initial history taken. “They are given a virtual reality goggle set to watch during the procedure, so part of the preparation is asking the child what show they want to watch,” says Dr. Mencin. “Then the child is brought over to the suite where they sit in a chair rather than lay back on a stretcher.”
Instead of receiving intravenous anesthesia, a local anesthetic is used in the nose and sprayed in the back of the throat, and then the procedure begins. “The parents are allowed to be in the room with the patient, so they’re participating in the care,” he says. “When I’m doing the procedure, I’m talking to the parent and to the patient and coaching them through the whole thing.”
Once the TNE is complete, the patient is brought to the recovery area where they stay for about 30 minutes. “They stay usually about a half hour or less, until the sensation comes back in the back of their throat, and they can swallow comfortably,” Dr. Mencin adds. “Then they can resume regular activities, including going right back to school.”
Will TNE Replace Traditional Esophagoscopy?
While unsedated TNE will play a big role in monitoring how disease treatment is progressing, it won’t replace traditional esophagoscopy entirely. “I would make the initial diagnosis with a standard scope with sedation but then I would feel comfortable using TNE to monitor response to therapy,” says Dr. Mencin.
The idea of doing this awake might be unsettling for some patients; however, Dr. Mencin says that the benefits far outweigh the trepidation. In terms of discomfort, because the nose is sedated, he says it’s not particularly uncomfortable. “I’ve done these to myself and had them performed on me,” he says. “Because the nose is anesthetized, it’s not that uncomfortable when the scope is going through. Patients are often concerned that they may gag during the procedure. However, after the topical anesthetic is applied the gag reflex is muted or disappears. Once the scope passes into the esophagus, you can still feel the scope, but it is not painful.”
Because the nose is anesthetized, it’s not that uncomfortable when the scope is going through. Patients are often concerned that they may gag during the procedure. However, after the topical anesthetic is applied the gag reflex is muted or disappears. Once the scope passes into the esophagus, you can still feel the scope, but it is not painful.
— Dr. Ali Mencin
Not everyone will be a good candidate for a TNE. “A good candidate is someone who is not very anxious. Having a nasogastric tube before and/or having used nasal sprays can make the procedure easier. ,” Dr. Mencin says. “Those are the best candidates. But I think that you don’t have to have done any of those things to do well with a TNE.”
Dr. Mencin sees TNE eventually becoming the gold standard for disease monitoring in EoE. The slim scope used in EoE could also have other uses such as feeding tube placements, evaluating for esophageal varices in children with portal hypertension, and could also be used in the hospital setting to determine the cause of abdominal symptoms such as pain or bleeding. “I believe that there are a lot of different applications,” he says. “The TNE platform is FDA approved for standard upper endoscopy, but the experience right now revolves almost exclusively around EoE; it could have much broader application.”




