Propelled by the urgent need for more effective treatments for anxiety disorders in youth, Francis Lee, MD, PhD, Chair of the Department of Psychiatry and Psychiatrist-in-Chief at NewYork-Presbyterian/Weill Cornell Medicine, and others at NewYork-Presbyterian/Weill Cornell Medicine are delving into the neurobiology of anxiety to personalize and optimize treatment to the state of the developing brain. Recently, the team discovered an alternative neurobiological pathway in adolescent mice and humans that elicits a strong response to safety signal learning, a potential therapeutic approach that forges an association between environmental stimuli and feeling safe.
Because of their explicit and specific association with safety, safety cues are capable of dampening the physiological and behavioral responses that normally arise when there is a perceived threat. The team is incorporating this novel intervention into a next-generation mobile app to broaden access to therapy in this vulnerable patient population.
“Adolescence is a time of dramatic neurodevelopment, as well as increased susceptibility to mental illnesses such as anxiety and depression, yet current treatments for anxiety, such as cognitive behavioral therapies (CBT), have largely been optimized for adults,” explains Dr. Lee. “Because adolescents have a less developed prefrontal cortex, therapies such as CBT that rely on this pathway may not be fully optimized for the developing brain.”
Adolescence is a time of dramatic neurodevelopment, as well as increased susceptibility to mental illnesses such as anxiety and depression, yet current treatments for anxiety, such as cognitive behavioral therapies (CBT), have largely been optimized for adults. Because adolescents have a less developed prefrontal cortex, therapies such as CBT that rely on this pathway may not be fully optimized for the developing brain.
— Dr. Francis Lee
“Exposure-based CBT, the primary behavioral treatment for individuals with anxiety is based on principles of fear extinction in which patients repeatedly and systematically confront fear-provoking stimuli with the goal to reduce anxiety. CBT has shown effectiveness in reducing anxiety symptoms however, up to 50% of treated youths have persistent anxiety symptoms,” says Dr. Lee.
Seeking New Approaches to Treating Anxiety in Adolescents
These findings suggest that patients with anxiety disorders may benefit from additional methods of fear reduction. One particularly promising approach is inclusion of a safety cue that would have a calming effect. Because of their explicit and specific association with safety the incorporation of safety signals may also enhance efficacy and tolerability. In this context. Lee and his team have been conducting research that explores the neural basis of safety signal learning using a vertically integrated research strategy to perform parallel mouse model studies and human behavioral and neuroimaging studies.
In 2019, the team led by Dr. Heidi Meyer utilized the cross-species research approach in a groundbreaking study that identified a common underlying neurocircuitry in both mouse models and humans for safety signal learning.
In the study, the team employed a variety of neuroimaging techniques to demonstrate that fear and anxiety in mouse models can be reduced using safety signal learning that relied on the hippocampus. The team’s collaborator, Dr. Dylan Gee, at Yale University used functional neuroimaging to confirm the same findings in humans given safety signals that the hippocampal-prefrontal cortical pathway was similarly engaged during safety signal learning.
“This study was one of the first to show that you can actually activate the hippocampus with safety signals to diminish fear and anxiety,” says Dr. Lee. “The study was also one of a few that used cross-species analyses to assess the actual neurobiological mechanisms that are involved in decreasing fear and anxiety.”
This study was one of the first to show that you can actually activate the hippocampus with safety signals to diminish fear and anxiety. The study was also one of a few that used cross-species analyses to assess the actual neurobiological mechanisms that are involved in decreasing fear and anxiety.
— Dr. Francis Lee
Later, in 2023, the team discovered that intermixing safety cues into extinction learning paradigms strengthened extinction memory in both adult and adolescent mice. The team also found adolescent mice are more efficient than adult mice in using safety signals, and that initial safety learning was actually faster in the adolescent mice. Thus, targeting a distinct pathway via safety signals may provide an effective alternative to enhance treatment for individuals for whom the efficacy of exposure-based CBT is otherwise limited.
“This research indicates that safety signal learning may be a developmentally appropriate way to design behavioral interventions for anxiety in adolescents,” says Dr. Lee. “In the clinical setting, incorporating safety signal learning may be used to bolster anxiety treatment during adolescence or used as an alternative for individuals who do not sufficiently benefit from typical interventions.”
This research indicates that safety signal learning may be a more developmentally appropriate way to design behavioral interventions for anxiety in adolescents. In the clinical setting, incorporating safety signal learning may be used to bolster anxiety treatment during adolescence or used as an alternative for individuals who do not sufficiently benefit from typical interventions.
— Dr. Francis Lee
Bolstered by these findings, the team is currently working on developmental and circuit-based treatment approaches for anxiety disorders that involve introducing learned safety cues that bypass the prefrontal cortex and engage the hippocampus early in therapy (Figure 1). The therapy would consist of safety cues selected by the patient.
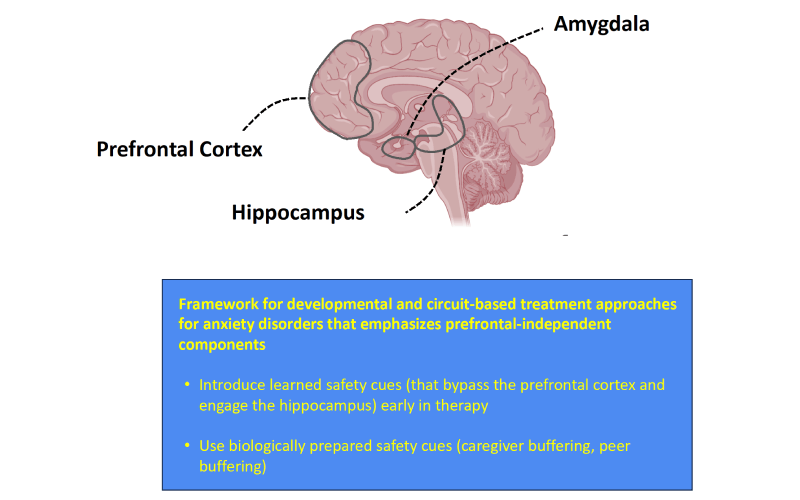
Developmental framework to guide potential treatment approaches for anxiety disorders.
With effective therapies on the horizon, Dr. Lee says the next challenge is to surmount the formidable barriers to provide access to therapy earlier in the disease process. “Adolescence represents the last window of heightened plasticity before neural systems reach a relative state of stability in the adult brain, yet less than two thirds of children and adolescents diagnosed with anxiety currently receive treatment,” explains Dr. Lee. “Moreover, despite the peak in diagnoses early in adolescence, treatment for anxiety is often not sought until several years later.”
Adolescence represents the last window of heightened plasticity before neural systems reach a relative state of stability in the adult brain, yet less than two thirds of children and adolescents diagnosed with anxiety currently receive treatment. Moreover, despite the peak in diagnoses early in adolescence, treatment for anxiety is often not sought until several years later.
— Dr. Francis Lee
A CBT Mobile App for Adolescents
To reach more adolescents with effective interventions, the team is collaborating with researchers led by Dr. Avital Falk at the NewYork-Presbyterian Center for Youth Mental Health to build a self-guided CBT app with safety signals incorporated into the app. “In the future, this self-guided app can be individually curated for each patient, who can customize it with their own safety signals,” says Dr. Lee. “Dr. Falk and her colleagues have just completed a randomized controlled clinical trial that measured effectiveness before and after exposure to the basic version of the app. Preliminary findings suggest that the app is just as effective as in-person CBT for people with mild to moderate anxiety.”
Because mobile apps are readily used by youth, this self-guided CBT app can be a familiar channel for assessments and treatment. “With this mobile app, patients can begin CBT while they are waiting for in-person treatment,” says Dr. Lee. “We are hopeful that the app will encourage more adolescents to begin and stay in treatment. “We know there is a certain level of resilience in the human brain,” says Dr. Lee. “Our goal is to help patients use apps like this to build their own “resiliency tool kit” that they can access whenever they perceive a situation as stressful.”
Looking toward the future, Dr. Lee is aiming to conduct foundational neuroscience research to determine exactly which sets of neurons in the hippocampus are involved in safety signal learning. Dr. Lee and his team are also continuing research to develop augmented safety signal modules within the CBT app. “NewYork-Presbyterian is the ideal setting to accomplish these challenging initiatives,” says Dr. Lee. “Here we have the infrastructure, such as basic neuroscience research labs and functional neuroimaging facilities, to conduct this research, and we also have some of the best clinical psychologists in the world to help us envision how to assess and deliver evidence-based treatments through digital CBT app platforms.”
NewYork-Presbyterian is the ideal setting to accomplish these challenging initiatives,” he says. “Here we have the infrastructure, such as basic neuroscience research labs and functional neuroimaging facilities, to conduct this research, and we also have some of the best clinical psychologists in the world to help us how to assess and deliver evidence-based treatments through digital CBT app platforms.
— Dr. Francis Lee
“The mobile app exemplifies what I hope will happen more in the field of psychiatry: taking findings from the bench to the bedside, and from the bedside to the community,” adds Dr. Lee. “I am thrilled that we are on this path of developing a personalized, targeted and accessible approach to treating anxiety in adolescents, which is essential to the well-being of this special population.”




