Read more about our top research and key innovations from 2023:
Cardiology & Heart Surgery
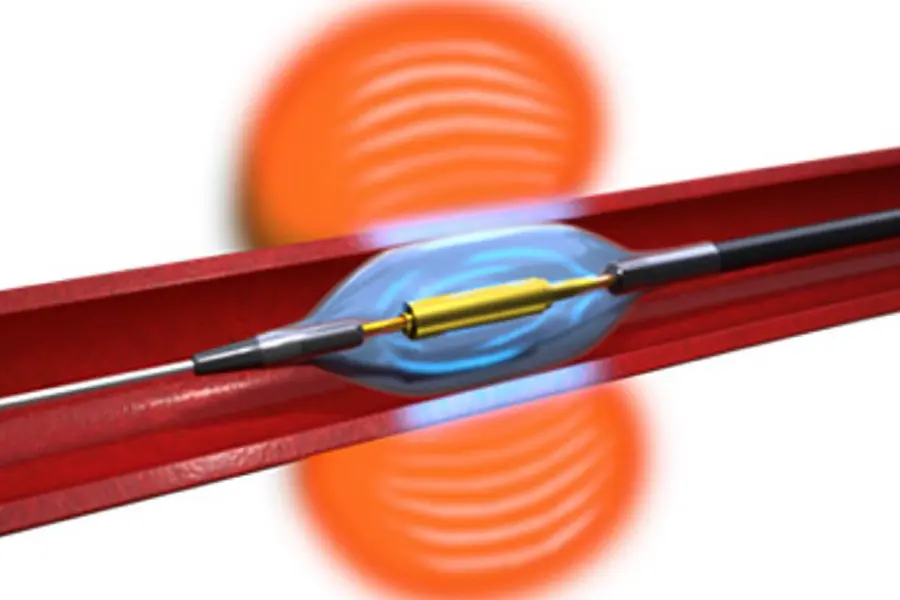
Treating Hypertension with Ultrasound Renal Denervation
Women Fare Worse Than Men Undergoing CABG: Time to Close the Gap
A Potentially Curative Procedure for CTEPH
The First-Ever Infant Domino Partial Heart Transplant
Neurology & Neurosurgery
Unlocking the Mysteries of Hidden Consciousness in Comatose Patients
The First 3D-Navigation-Guided Endoscopic TLIF in NYC
Oncology
Targeted Treatment for Metastatic Gastric Cancers Extends Survival
Focused on Detecting and Preventing High-Risk GI Cancers
Treatment for Gastric Cancers Extends Survival
Orthopedics
Breakthrough Shoulder Prosthesis Promises Improved Outcomes
Novel Approaches to Periprosthetic Joint Infections
Advances Across All Medical Specialties
Testing a Revolutionary Pathway to Achieve Tolerance in Kidney Transplantation
Novel Brain Study Uncovers Autism Subtypes
A Pilot Study: Can a Weekly Pill Slow Ovarian Aging and Delay Menopause?
Advancing RNA-based Vaccines for Cancers Associated with Lynch Syndrome